Stem Cell Research Associated with Obesity
Ashlyn Thomas1 and Vincent Gallicchio2*
1,2Department of Biological Sciences, College of Science, Clemson University Clemson, SC 29627, USA.
*Corresponding author: Vincent Gallicchio, 2Department of Biological Sciences, College of Science, Clemson University Clemson, SC 29627, USA.
Citation: Thomas A, Gallicchio V. J Stem Cell Res. Stem Cell Research Associated with Obesity. 5(1):1-11.
Received: May 14, 2024 | Published: May 27, 2024
Copyright© 2024 genesis pub by Thomas A. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation
DOI: https://doi.org/10.52793/JSCR.2024.5(1)-58
Abstract
Obesity has become a prevalent concern that is characterized by adipocyte hypertrophy and hyperplasia, adipose tissue inflammation, and insulin resistance. Side effects of this condition include the development of type 2 diabetes, non-alcoholic fatty liver disease, cardiovascular disorders, osteoarthritis, and osteoporosis. Obesity onset is due to a combined set of factors including behavioral, biological, environmental, genetics, and socioeconomics. Treatments for obesity currently include increasing exercise and decreasing food intake to create a net negative energy balance. This helps to burn more calories than calories consumed which leads to decreasing weight overall. Other interventions include bariatric surgeries to reduce large amounts of fat mass and pharmacological treatments. However, weight regain is typical for these types of management, and can even lead to more weight gain than prior to starting treatment. By utilizing stem cells, a potential new and more effective treatment may help to improve this epidemic and can aid in decreasing obesity rates across the world.
Keywords
Obesity; Adipose-Derived Stem Cells (ADSC); MSC (Mesenchymal stem cells); Metabolic Subcutaneous
List of Abbreviations
ADSC - Adipose-Derived Stem Cells; MSC - Mesenchymal Stem Cells; AD-MSCs - Adipose-Derived Mesenchymal Stem Cells; WHO - World Health Organization; PwO - People with Obesity; BMI - Body Mass Index; COVID-19 - Coronavirus Disease 2019; BAT - Brown Adipose Tissue; AIP - Atherogenic Index of Plasma; ND - Normal Diet; HFD - High Fat Diet; HbA1c - Hemoglobin A1c; HMSCs - human mesenchymal stem cells.
Introduction
Obesity is an ongoing condition that leads to many metabolic diseases as it is increasing worldwide and has doubled for men and women between 1980 and 2016. It is expected that by 2030, 57.8% of the global population will be obese [1]. Nearly 2 billion adults are overweight or obese internationally. This condition has been deemed a global epidemic and due to its role in being related closely to metabolic diseases, the need to treat it efficiently and effectively is significant [2]. Therapeutic intervention using stem cells have become a staple in helping manage this prevalent second leading cause of preventable death. Obesity is a public health concern that contributes to 4.7 million premature deaths per year and continues to increase dramatically. This condition can cause metabolic issues including type 2 diabetes, hypertension, dyslipidemia, cardiovascular disease, non-alcoholic fatty liver disease, and fertility problems [3]. Therefore, obesity itself contributes to a wide variety of other health-related diseases as well. This makes it necessary to find new interventions to prevent and treat it to minimize other health-related conditions associated with obesity.
Pathology
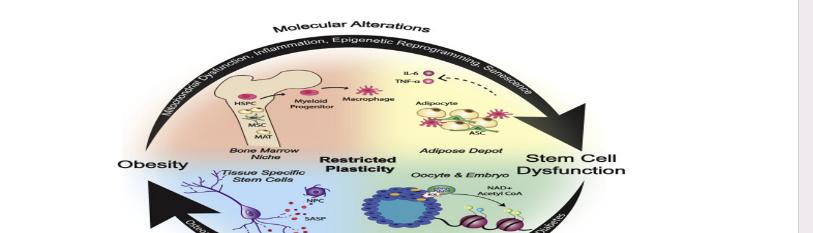
Obesity is the abnormal accumulation of fat because of more caloric input compared to output from adipose tissue of subcutaneous fat distributions [4]. It consists of a chronic illness with the calorie intake exceeding the calorie expenditure. This fat gain from the positive net addition is stored as excess fat [5]. Obesity is a result of calorie utilization, increased appetite, and lack of physical activity. It is the state of excessive malnutrition and can lead to other defective systems in the body. More fat is being stored than expressed or used up which accumulates over time (figure 1).
Figure 1: The mechanism of metabolic syndrome caused by obesity. Abdominal fat accumulates and produces excess free fatty acids. The increased oxidation rates of free fatty acids inhibit binding of hepatic insulin receptors to insulin which aids in insulin resistance [6].
Figure 2: The correlation between ADSCs and obesity onset. ADSCs can help to maintain physiological function of fat cells [6].
Onset of Obesity
Obesity is characterized by increased body mass resulting from growth of fat tissue. Patients with obesity are at risk for other health problems including type 2 diabetes, high blood pressure, heart disease, high total cholesterol and triglycerides, stroke, sleep apnea, and certain types of cancer [7]. For instance, other studies show that older age of obesity onset may be a major factor in determining the risk of developing weight-related diabetes. Determinants that influence obesity include eating and physical activity patterns, and insufficient sleep. Social determinants also play a role as it can be difficult to make healthy food choices and get enough exercise if those around an individual do not support those health choices. Different socioeconomic groups can continue to do this as not all people have the funds for transportation or to buy healthy foods as they tend to be more expensive. Genetics can play a role as variants in several genes can contribute by causing an increase in hunger and food intake. However, it rarely occurs that a specific gene (monogenic obesity) causes a clear pattern of inherited obesity within a family [8, 9]. Certain illnesses may contribute to the onset of obesity like Cushing’s disease. Drugs including steroids and some antidepressants can cause weight gain. Suggestions related to chemical exposures and the role of the microbiome may be a factor and related as well.
Hormone Influence on Obesity
Many hormonal influences are associated with obese conditions. Obesity is associated with endocrine alterations including hypothyroidism, Cushing's disease, hypogonadism, and growth hormone deficiency [10]. The weight gain leading to onset of obesity from increased energy intake may result from the body not properly matching burned versus consumed calories. Many hormones are continuously on the rise for having a contribution in energy balance and food intake. Many functions of adipose tissue are regulated by hormones and released by adipocytes. The peptide hormone leptin can cross the blood-brain barrier and attach to neurons of the hypothalamus which helps to mediate appetite and energy expenditure. It can signal lack of food intake and decrease when the body is in a fasting or low-calorie state. Obesity is associated with sex hormones and can influence expression of obesity phenotypes.
There is evidence that subclinical alterations may be a cause for increased adiposity leading to obesity. There is a major correlation between the body and adipose tissue. For example, there are endocrine syndromes that are known to result in obesity. Diseases including hypothyroidism, Cushing’s syndrome, hypogonadism, and growth hormone deficiencies are all associated with abdominal obesity [11]. Estrogen is a common hormone that stores fat for reproduction and can lead to weight gain as well. Keeping this hormone at normal levels is necessary to prevent the onset of obesity. Stem cells can help cue hormones to allow them to coordinate more properly with the body and its reaction to physiological changes.
Current Standard of Care
It is not effectively managed in our current health systems. There is a lack of knowledge and experience with hot to support obese patients. Biased beliefs about this condition also contribute to the level of quality of care for patients who are obese. This results in healthcare providers portraying acts of blame upon those with obesity due to perceived lack of will power and personal choices. Providers may immediately assume that patients are fully willing to manage their weight and oftentimes do not ask permission to discuss the condition with their patient. There is a lack of interdisciplinary programs to manage the health of obese patients, long wait times for referrals, appointments, and surgery, and high costs for treatments [11]. There are not enough physicians with obesity qualifications and expertise to treat patients with this condition. Current treatment options besides surgery, do not yield weight loss beyond 20% which may even make little effect on health improvements for many obese patients. In practice, nearly 25% of PwO achieve an annual weight loss ≥5%. According to the Awareness, Care and Treatment in Obesity Management—an International Observation (ACTION-IO) study, only 12% of PwO reported a loss of at least 10% of body weight over the past 3 years [12]. Overall, less than half of the group in this study was able to maintain their weight loss for at least 1 year. To conclude, there is little information on successful long-term strategies to precede weight regain which may make a patient’s efforts to lose weight feel pointless.
The American College of Cardiology, American Heart Association, and Obesity Society have published guidelines recommending adults to be screened annually using a body mass index (BMI) measurement (body weight [kg]/height [m2]) to evaluate weight patterns. They concluded that A BMI of 30 kg/m2 to 34.9 kg/m2 defines class 1 obesity of between 35 kg/m2 and 39.9 kg/m2 constitutes class 2 obesity, and of at least 40 kg/m2 marks class 3 obesity [13] (Figure 3).
Figure 3: WHO guidelines used these classes to indicate a patient’s risk of weight-related disease including mild, moderate, and severe. This is based on the individual's body mass index which measures their height and weight [14].
Why current treatments are not effective?
Education in obesity and nutrition are not presented adequately or properly in undergraduate criteria. There is a lack of training for health professionals on obesity significance. There is also a lack of a formal diagnosis of obesity. Little time during general practice and consultations contributes to barriers for management as well. Endoscopic interventions work on various mechanisms but are limited by the fact that they are only made for a definite period and require removal only offering temporary benefits. Increases in harmful behaviors and suicide risks have been reported amongst bariatric surgery patients. Possible hypotheses for this include the alterations in absorption of medications, peptide or hormone imbalances, and post-operative eating disorders due to changes in eating habits to be considered a good candidate for the bariatric surgery [13]. This surgery can result in nutritional deficiencies which may require lifelong supplements. Dumping syndrome results from complications of specific bariatric surgeries arising from rapid gastric emptying. Early dumping within 30 minutes following a meal has symptoms including pain, bloating, diarrhea, and borborygmi [15]. Late dumping following a meal 1-3 hours is correlated with hypoglycemia and has shown symptoms including dizziness, fatigue, sweating, and weakness [15]. Evidence shows revision and reversal of bariatric surgery may be feasible and can result in complications of their ongoing intolerant symptoms. Many people seek information from alternative sources including the internet, family friends, television programs, and smartphones as compared to health care providers. Successful weight loss may depend on how a patient’s environment functions including their support system which may not be permanently implemented. Low socioeconomic status may contribute to the lack of care patients are willing to pay to manage their weight better. Other costly factors include the high costs of food, and high weight loss programs or gym membership monthly rates make it more difficult to encourage healthier lifestyles [13] To continue, many medications to help treat obesity are not reimbursed by health care systems or insurance [16]. Many people themselves do not understand the chronic disease obesity is and the relapse effects it causes if not managed and maintained properly [13].
Why stem cell use is important?
Several studies have shown that ADMSCs help to improve pancreatic islet cell viability and function, hyperglycemia, and insulin sensitivity. They can also aid in restoring liver function, reverse dyslipidemia, lower pro-inflammatory cytokines, and reduce oxidative stress in animal models. Mesenchymal stem cell (MSC) therapies have been proposed to influence adjunctive therapy for obese patients which may help reduce economic burdens of treatment through prevention and proper management of stem cells through an individual’s life [17]. Due to their adipogenesis role they propose an attractive alternative for weight management of obese patients including their relative ease of isolation and expansion coupled with their immunomodulatory and anti-inflammatory and homing properties [18]. The mesoderm produces stem cells called progenitor cells which can self-renew and multi-direct differentiation including bone, fat, and chondrocytes. ADSCs utilize easy access, rapid proliferation, and autologous transplantation [6].
Stem Cells being Investigated for the Intervention of Obesity-Related Conditions
-
Adipose‐derived mesenchymal stem cells (ADMSCs)
-
Bone marrow derived MSC
-
Induced pluripotent stem cells
-
Human embryonic stem cells
Clinical studies performed in humans
Recent evidence suggests that cells with the properties of human mesenchymal stem cells (hMSCs) can be derived from adult peripheral tissues, including adipose tissue, muscle, and dermis [18]. Isolation of hMSCs from the vascular portion of subcutaneous adipose tissue from seven adult subjects (two men and five women) has been used. ADMSC‐based clinical trials have grown over the years largely due to their abundance, ease of isolation, rapid expansion, high proliferation capacity, and no ethical issues [18]. It was found that ADMSCs isolated from patients with obesity have a lower proliferative and differentiation capacity and therefore are less effective in immunomodulation compared with lean, metabolically healthy individuals. ADMSCs therapy is beginning to gain more attraction for obese-related cases. Although studies performed in humans may be limited per ethical dilemmas, there are some that can be used to evaluate the impact of stem cell use for obesity. More human studies are needed to better evaluate the need for stem cells when treating obesity.
Results of Animal Studies using Stem Cells in an Animal Model with Obesity
Using obese rats, it was observed that the accumulation of adipose tissue cells into fatty cysts were correlated with excessive accumulation of fat like those fat accumulations formed in the liver from hepatic cells [19]. One study used C57BL6 mice for their experiment and fed them a high fat diet (HFD) or the CHOW diet which consists of a grain-based diet for 15 weeks. Obese and lean mice were given two doses of AD-MSCs. The treatment using these stem cells reduced blood glucose levels, HbA1c and AIP. They increased glucose tolerance in pre diabetic mice. To continue, the MSCs reduced levels of inflammatory mediators in mice fed high fat diets. They were also effective in preventing cardiovascular diseases. After injection of these stem cells, the percentages of fat mass decreased significantly in the HFD group. This study utilized human cells compared to murine MSCs in animal disease models to more closely mimic patients and accelerate the translation of stem cell therapy to clinical practice [20].
Another study using a similar method with mice and HFD found the content of ADSCs in the subcutaneous adipose tissue increased. However, its telomerase activity decreased, the length of telomeres was shortened, and proliferation ability was weakened. Therefore, the self-renewal ability of ADSCs from obese patients was decreased [6] (Figure 4).
Figure 4: This shows how ADSCs contribute to treatment of obesity and the results it leads to. They aid in direct repair of damage, anti-inflammatory responses, cell protection, anti-apoptosis, and immune regulation [6].
Figure 5: MSC treatment reduces the atherogenic index of plasma (AIP) in obese mice. AIP was measured at the end of the study in ND- and HFD- fed mice treated and untreated with AD-MSCs. n = 6, ***p < 0.001 [18].
Current Future Endeavors
More research is still needed to assess AD-MSCs transplantation regarding treating obesity in humans globally [18]. More experiments should be made to answer questions including: What dosage, frequency, timing of transplantation, and transplantation route can achieve the best therapeutic effect? Stem cells that enter the blood circulation, especially stem cells transplanted through the venous system, will be trapped by other organs before attaching to the target cells. What is the ratio of trapped stem cells? How long can they stay after reaching the target organ? What is the long-term effect?
There is still limited evidence to support if stem cell transplantation can improve the accumulation of abdominal fat. Although studies using adipose tissue from rodent models have been beneficial, there is still a lack of comparison to humans due to the major physiological component differences between humans and animals. For example, the origin, identity, and heterogeneity of brown adipose tissue (BAT) are different amongst mouse models compared to humans. The activity of human BAT utilized the β2 adrenergic receptor, whereas the β3 adrenergic receptor is used in mice [21].
Mice are also typically kept below tempturates that humans usually live in. There is a significant need for maturing human adipocytes or organoid systems to model different cell types within adipose tissue. This will help create more evidence and strategies to treat adipose-related metabolic diseases including obesity [22]. There is scarcity of suitable preclinical human models. iPSC technology has bypassed ethical concerns around using hESCs that are derived from human embryos. This encompasses patient-specific pluripotent stem cells, which provide a foundation for drug discovery and cell therapy [23]. More 3D culture systems should be used to continue the differentiation between visceral and subcutaneous preadipocytes into mature adipocytes to retain gene expression, thermogenesis, lipolysis, and cytokine secretion [24]. Diverse immune cells are necessary as adipose tissue is highly heterogeneous that consists of adipocytes, connective tissue, vasculature, immune cells, and nerves [25]. Intervention of sympathetic nerve fibers may contribute as they control adipocyte lipolysis and thermogenesis through noradrenaline secretion. Developing adipose organoids and inducing browning of this tissue may be used as a treatment of obesity in the future [26].
Conclusion
Obesity is a critical condition that has increased in rates drastically becoming an epidemic. It arises from an onset of multiple factors including the environment, biological, behavioral, social, and genetics. Current treatment options including changes in diet and exercise routines, and pharmacological and bariatric surgery interventions have shown little improvement in decreasing the prevalence of obesity. Therefore, it is crucial to implement a new treatment with stem cells, specifically adipose-derived mesenchymal stem cells, to decrease obesity and the health-related diseases associated with it. Treatment observed and experimented with in mice has shown positive results for treating obesity and decreasing health-related conditions including insulin resistance, glucose intolerance, hyperlipidemia, and inflammatory diseases. COVID-19 also played a major role in how it affected obese patients, bringing attention to the condition in more depth. As many people had to quarantine, physical activity and availability of healthy foods became limited quickly and further increased obese rates. Because of these impacts on the health of humans and the increased rates of obesity, it is crucial to find alternative methods to treat obesity and related diseases. Although more stem cell research is needed to increase accuracy and support for its effectiveness on treating obesity, it is a step in the future for treating obesity.
References
- Mansoor S., Hameed A., Anjum R., Maqbool I., Masoodi M., Maqbool K., Dar Z. A., Hamadani A., Mahmoud A. E. D. (2021). 21 - Obesity: Causes, consequences, and disease risks for service personnel. In Phytochemistry, the Military and Health. 407-25.
- Guerra JV, Dias MM, Brilhante AJ, Terra MF, Garcia-Arevalo M, et al. (2021) Multifactorial basis and therapeutic strategies in metabolism-related diseases. Nutrients. 13(8):2830.
- Hruby A, Hu FB. (2015) The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics. 33(7):673-89.
- Panuganti KK, Nguyen M, Kshirsagar RK. Obesity. [Updated 2023 Aug 8]. In: StatPearls [Internet].
- Schutz Y. (1995). Macronutrients and energy balance in obesity. Metab Clin Exp 44:7-11.
- Yang H, Li C, Li Y, Tai R, Sun C. (2021) Adipose-derived stem cells and obesity: The spear and shield relationship. Genes Dis. 10(1):175-86.
- Fruh SM. (2017) Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract. 29(S1):S3-14.
- Yanovski SZ, Yanovski JA. (2018) Toward Precision Approaches for the Prevention and Treatment of Obesity. 19(3):223-4.
- Qasim A, Turcotte M, Samaan MC, Champredon D, Souza RJD. (2018) On the origin of obesity: identifying the biological, environmental and cultural drivers of genetic risk among human populations. 19(2):121-49.
- Ylli D, Sidhu S, Parikh T, et al. Endocrine Changes in Obesity. [Updated 2022 Sep 6]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
- Dietz WH, Baur LA, Hall K, Puhl RM, Taveras EM, et al. (2015) Management of obesity: improvement of health-care training and systems for prevention and care. The Lancet. 385(9986):2521-33.
- Kim TN. (2020) Barriers to Obesity Management: Patient and Physician Factors. J Obes Metab Syndr. 29(4):244-7.
- Cornejo-Pareja I, Clemente-Postigo M, Tinahones FJ. (2019) Metabolic and endocrine consequences of bariatric surgery. Frontiers in endocrinology. 10:439786.
- Anilkumar B. (2017) A Comparative Study of Prevalence and Risk Factors of Overweight and Obesity Among Male and Female MBBS Students in KVG Medical College and Hospital, Sullia, DK, Karnataka (Doctoral dissertation, Rajiv Gandhi University of Health Sciences (India)).
- Masclee GMC, Masclee AAM. (2023) Dumping Syndrome: Pragmatic Treatment Options and Experimental Approaches for Improving Clinical Outcomes. Clin Exp Gastroenterol. 16:197-211.
- Kim N, Estrada J, Chow I, Ruseva A, Ramasamy A, et al. (2023) The Relative Value of Anti-Obesity Medications Compared to Similar Therapies. Clinicoecon Outcomes Res. 15:51-62.
- Mikłosz A, Nikitiuk BE, Chabowski A. (2022) Using adipose-derived mesenchymal stem cells to fight the metabolic complications of obesity: Where do we stand? Obes Rev. 23(5):e13413.
- Jaber H, Issa K, Eid A, Saleh FA. (2021) The therapeutic effects of adipose-derived mesenchymal stem cells on obesity and its associated diseases in diet-induced obese mice. Sci Rep. 11(1):6291.
- Sampey BP, Vanhoose AM, Winfield HM, Freemerman AJ, Muehlbauer MJ, et al. (2011) Cafeteria diet is a robust model of human metabolic syndrome with liver and adipose inflammation: comparison to high‐fat diet. Obesity. 19(6):1109-17.
- Dicker A, Le Blanc K, Aström G, van Harmelen V, Götherström C, et al. (2005) Functional studies of mesenchymal stem cells derived from adult human adipose tissue. Exp Cell Res. 308(2):283-90.
- Paul Lee, Michael M. Swarbrick, Ken K. Y. Ho, Brown Adipose Tissue in Adult Humans: A Metabolic Renaissance, Endocrine Reviews. 34(3):413-38.
- Hu W, Lazar MA. (2022) Modeling metabolic diseases and drug response using stem cells and organoids. Nat Rev Endocrinol. 18(12):744-59.
- Moradi S, Mahdizadeh H, Šarić T, Kim J, Harati J, et al. (2019) Research and therapy with induced pluripotent stem cells (iPSCs): social, legal, and ethical considerations. Stem Cell Res Ther. 10(1):341.
- Dicker A, Le Blanc K, Aström G, van Harmelen V, Götherström C, et al. (2005) Functional studies of mesenchymal stem cells derived from adult human adipose tissue. Exp Cell Res. 308(2):283-90.
- Michailidou Z, Gomez-Salazar M, Alexaki VI. (2022) Innate Immune Cells in the Adipose Tissue in Health and Metabolic Disease. J Innate Immun. 14(1):4-30.
- Shamsi F, Wang CH, Tseng YH. (2021) The evolving view of thermogenic adipocytes—ontogeny, niche, and function. Nature Reviews Endocrinology, 17(12):726-44.

