Protein Receptors on Chondrocytes
Gordon Slater1*, Samar Javadian2
1Orthopaedic Surgeon, Private Practice, Level 2, Suite 2.01,376 New South Head Rd, Double Bay, NSW 2028; Australia
2Master of Biotechnology, Australia
*Corresponding author: Gordon Slater, Orthopaedic Surgeon, Private Practice, Level 2, Suite 2.01,376 New South Head Rd, Double Bay, NSW 2028; Australia
Citation: Slater G, Javadian S. (2021) Protein Receptors on Chondrocytes. J Stem Cell Res. 2(2):1-10.
Received: March 31, 2021, | Published: April 15, 2021
Copyright© 2021 genesis pub by Slater G, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License., This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/JSCR.2021.2(2)-19
Abstract
Here we reviewed various protein receptors and their roles on chondrocytes. In connection with this we summarized that GPCRs, VEGF receptors, integrins, TLRs, LRP receptors, chemokine receptors and growth factor receptors are the main receptors on chondrocytes. We have discussed different receptors involved in chondrocyte differentiation and those activating proliferation in chondrocytes. We conclude that among the myriad of protein receptors expressed by chondrocytes, some (TLRs, LRPs and chemokine receptors) have the important role in osteoarthritis (OA). These receptors could be targeted by pharmaceutical agents to treat intra-articular injuries including osteoarthritis.
Keywords
Chondrocytes; Protein receptors; Osteoarthritis; ECM; Differentiation; Inflammation; Slater
Introduction
Chondrocytes are critical cells in the extracellular matrix (ECM) of articular cartilage. The plasma membrane of articular chondrocytes is comprised of varied membrane proteins such as channels, transporters, enzymes, receptors, and anchors for intracellular, cytoskeletal and ECM proteins and other macromolecular complexes which determine the cell surface phenotype of the cells (Figure 1). Interestingly membrane proteins are valuable pharmaceutical targets and are crucial for chondrocyte function [1,2]. This review details the myriad of studies of protein receptors on chondrocyte and high-light the need for further, more-comprehensive research to validate clinical receptors-based approaches towards diseases.
Figure 1: Distribution of the surface proteins on chondrocytes is identified in this study. One hundred proteins were classified as enzymes (23%), 128 proteins had receptor roles (30%), 51 proteins were involved in transport processes across the PM (12%), 120 proteins were involved in adhesion, cell-cell or cell-matrix junctions and cytoskeletal organisation (28%), and 20 proteins were structural ECM components (5%). Ninety-four proteins (22%) could not be assigned to one of the subgroups or their function was unknow.
G-protein coupled receptors (GPCR)
G-protein coupled receptors (GPCR), a large family of seven-transmembrane domain receptors, which consists of alpha, beta and gamma subunits [3], appear to contribute to exhibit bone expression, [4]] and control the proliferation, differentiation, and apoptosis of osteoblasts, osteoclasts, and chondrocytes by GPCR signalling [5].It seems that not only is Gαs a major participant in chondrocyte differentiation, but also it inhibits the differentiation process. The observations reported herein that the absence of Gαs in fetal [6] or postnatal [7] chondrocytes conduces to considerable stimulation of chondrocyte differentiation and termination of longitudinal bone growth. Alternatively, an isoform of Gαs (XLαs), with an alternative exon 1, is capable of initiating the downstream cyclic AMP (cAMP) signalling pathway [8], which suppresses markers of hypertrophic chondrocytes such as ALPase activity and collagen type X expression in differentiated cultured rabbit chondrocytes [9]. There are several GPCRs expressed by chondrocytes activating Gαs which controls chondrocyte hypertrophy. These include PTHR1 [10], receptors for prostaglandins [11,12], membrane estrogen receptor GPER [9], RDC1 receptor [13], adenosine (nucleotide P2Y) receptors [14,15], β-adrenergic receptors [16], histamine H2 receptors [17]. Although the absence of PTHR1 leads to a marked decrease in chondrocyte proliferation, and ectopic apoptosis of stemlike chondrocytes, effect of Gαs ablation was not observed upon [9]. On the other hand, pharmacological in vitro activation of PKC, the main downstream signalling pathway of Gq/11, promotes chondrocyte differentiation [17,18].Gq/11 can prevent apoptosis in the absence of Gαs, whereas it contends with its action to suppress differentiation in the presence of Gαs [19].There is evidence that the ablation of Rac1 (as a member of the Rho family of small G proteins) in chondrocytes, has been found to cause hypocellularity, decreased proliferation and growth retardation [20]. Particularly, Gi that is activated by chemokine receptors of chondrocytes [21], inhibits the cAMP pathway, and opposes Gαs action [22], which would increase chondrocyte differentiation. Given that Gαs can be activated by PTHR1, it has a crucial role to prevent premature chondrocyte differentiation and absence of either one causes instantaneous chondrocyte differentiation [19]. PTH/PTHrP receptor mRNA is highly expressed in maturing chondrocytes, while its expression is not observed in premature or fully hypertrophic chondrocytes. There is striking observation that GPR30 (a G protein-coupled estrogen receptor) has been detected in the resting and hypertrophic zones, and is not exhibited in the proliferative zone, which demonstrates that GPR30 is possibly responsible for chondrogenesis[19]. We found clear evidence of the impact of RDC1 (a class A orphan G-protein coupled receptor) not only on the expression of the genes correlated with chondrocyte hypertrophy but also on increased matrix degradation and the factors of OA development [23]. Additionally, RDC1 activation leads to an induction of MMP13 [24], which is highly upregulated in disease and leads to cartilage degradation[25]. Intriguingly, PGE2 (Prostaglandin E2) binds to one of four receptor isoforms, EP1,EP2, EP3, and EP4 which are coupled to G-proteins. The presence of EP-1 and 2 receptors was confirmed in rat growth plate chondrocytes [26,27] and EP4 receptors have been found in bovine articular chondrocytes [12]. EP1 is in consistent with Gq and promotes IP3 signalling and calcium transients [28]. Obviously, EP2 and EP4 associate with Gas and stimulate cAMP/PKA/CREB signalling which interfere in progression of chondrocyte differentiation [28,29], WhereasEP3 with EP2 and/or EP4 can downregulate activation of the cAMP/PKA/CREB cascade[28,29]. It has been found that an increase in EP4 and a decrease in EP3 receptor expressions occur through later stages of chondrocyte maturation [30,31]. The experiment consistently showed the existence of P2 receptors (a family of G protein-coupled receptors) namely P2Y2 as an agent of interleukin (IL)-1 secretion [41], P2X2 and P2X5 [14]on chondrocytes [32]. Histamine receptors as another class of G protein–coupled receptors in chondrocytes, which noticeably increase cAMP while decreasing KS (keratin sulfate) [33], could be expressed during the development of arthritis [34]. In particular, a variety of glutamate receptors have central role in bone remodelling [35-37]. One of these receptors is named calcium-sensing receptor (CASR) that its gene (Casr) knockout in chondrocytes interestingly suppresses embryonic development and cartilage maturation [38].
VEGF-receptors
Chondrocytes are exposed to an inflammatory micro-environment in the extracellular matrix (ECM) of articular cartilage in joint diseases such as osteoarthritis (OA) and rheumatoid arthritis (RA). The findings revealed that hypertrophic chondrocytes release angiogenic factors including VEGF, which is assumed to increase inflammation as well as its obligatory role for endochondral ossification [13]. Accumulating evidence suggests that VEGF-R1, VEGF-R2, VEGF-R3 and neuropilin-1 are expressed in osteoarthritic cartilage where chondrocytes demonstrate developmental differentiation [39,40]. Clearly, primary chondrocytes express three receptors for VEGF (neuropilin-1, VEGF-R2 and VEGF-R3), signifying that some VEGF might have a role in chondrocyte metabolism. Given VEGF-R2 (which bind VEGF-A and VEGF-C [41]) is expressed and stimulated by chondrogenic treatment, it implies that VEGF-A and VEGF-C may directly affect mature chondrocytes.
Integrins
Extracellular matrix (ECM) proteins affect cell proliferation, differentiation, and morphogenesis [42]. Integrins are heterodimeric transmembrane molecules composed of an α- and a β-subunit. Several observations suggest that the interaction between chondrocytes and matrix proteins is mediated by the β1 subfamily of integrins [43]. integrins interact with growth factors which might be important for cell adhesion, differentiation, growth, and survival in different cell types [44]. Additionally, Insulin-like growth factor I (IGF-I) which is identified to stimulate differentiation in chondrocytes [45,46], associates with β1 integrin in the chondrocyte adhesion to collagen type II[47]. Moreover,it has revealed that chondrocytes express the α1β1, α2β1, α3β1, α5β1, α6β1, α10β1, αvβ3, and αvβ5 integrins [48-53]. Indeed, α5β1 integrin, as the primary chondrocyte fibronectin (FN) receptor [45],is thought to be an important chondrocyte integrin accompanied with less expression of α1β1 and α3β1. Whilst, adult human chondrocytes have demonstrated the expression of α1β1, α5β1, and αvβ5 integrins compared to the less expression of α3β1 and αvβ3. Importantly, fetal chondrocytes and chondrosarcoma cells have higher expression levels of α2β1 and α6β1 integrins when Compared to adult chondrocytes [54,55]. Not only does the α1β1 integrin lead to adhesion of chondrocytes to type VI collagen [56], but also it mediates adhesion to cartilage matrix protein (matrilin-1) [57].
TLRs
According to the previous research, chondrocytes express TLR1, TLR2, and less TLR9. TLR is highly dependent on the activation and differentiation state of the chondroid cells, for instance, the involvement of TLR9 is deciphered in inflamed (OA) chondrocytes, but far less in mature, resting chondrocytes [58]. In contrast, the expression of TLR-4 is shown in human articular chondrocytes on both the messenger RNA (mRNA) and protein level [44]. Fascinatingly, TLR-7 was only apparent in chondrocytes among patients younger than age 35 years, implying that a patient’s age may influence TLR expression [59].
LRP receptors
Despite a large body of evidence demonstrating the role of LRP receptors (lipoprotein receptor-related proteins) in musculoskeletal homeostasis, LRP5 and LRP6 are critical for transmitting of canonical Wnt-signaling [60] which is linked with Cartilage and bone through processes such as endochondral ossification. Prior research highlights that in active Wnt-signaling, Wnts bind to the lipoprotein receptor-related protein (LRP) co-receptors [61]. Not only are LRP4, LRP5, and LRP6 within canonical Wnt-signaling regulated in simulated microgravity and cyclic hydrostatic pressure, but also these ones appear to contribute to cartilage degeneration[62].In addition, LRP5 has been found to be upregulated in osteoarthritis[63],whereas LRP6 loss-of-function mutation has been along with an enhanced progression of osteoarthritis [64].
Growth factors receptors
As has been previously reported in the literature, chondrogenic growth factors such as insulin-like growth factor (IGF)-1 and transforming growth factor (TGF)-β1 have influence on chondrogenic redifferentiation as well as the expression of Col2 and GAGs in the cartilage tissue [65]. Nevertheless, IGF-1 which Its activity is mediated via IGF-1 receptors (IGFR1) [66],is a major factor for chondrocyte proliferation and matrix synthesis [23]. Not only is the TGF-β1 a primary stimulator of proteoglycans and Col2 synthesis in chondrocytes [67],but also it is able to induce the chondrogenic differentiation of mesenchymal stem cells in vitro [68]. Signals are transferred by forming complex dimers of TGF-β receptor 1 (TGFBR1) and 2 (TGFBR2) [69]. Provided a deficiency of TGFBR1 occurs, stimulation of TGF-β1 in chondrocytes is improved by upregulation of TGFBR1. Furthermore, the higher expression of TGFBR2 under IGF-1 stimulation could also be Possible, due to a lack of the TGF-β1 in chondrocytes [70].
Chemokine receptors
As has been previously reported in the literature, chondrocytes also express chemokine receptors including CXCR3, CXCR4, CXCR5, CCR1, CCR3, CCR5 and CCR6 and several chemokines, namely IL-8, MIP-1α, GROαβγ, MCP-1, eotaxin-1 and RANTES, which might play significant roles in chondrocyte hypertrophy [71-72]. Undoubtedly, inappropriate activation of the chemokine network leads to inflammatory arthritis. For example, numerous chemokines are generated in joint tissues of patients with OA and after joint injury [73-74]. Research has provided evidence for the expression of CCL19 and its receptor CCR7 which is consistent with enhanced symptoms in the synovia of patients at an early stage OA [74]. Moreover, improved levels of CCL5 and CCL19 have been observed in synovial fluids derived from patients with both RA and OA [75-79].
Discussion
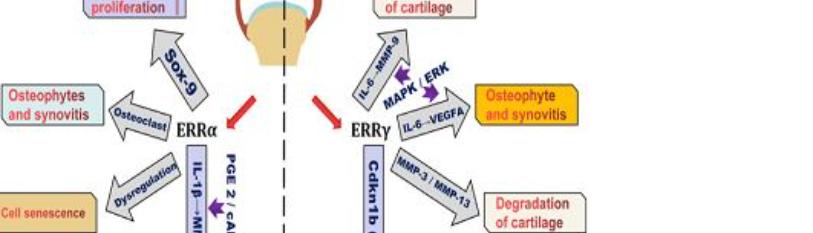
In summary, chondrocyte degradation as a process of ageing, disease and injury has a significant impact on everyones life. Chondrocyte biology is a controversial and emerging science. This article aimed to collect the recent research about chondrocyte proliferation, differentiation, and death and the pathogenesis of OA. Among all the protein receptors expressed by chondrocytes, RDC1, Histamine receptors, TLR9, LRP5, LRP6, CCR7, CCR7 have the most important role in OA development, whereas VEGF-R, β1 integrin, EP and Gi are the major activators of chondrocyte differentiation. It is believed that CASR and PTHrP have an important role in chondrocyte maturation, whilst IGFR1 and Rac1 seem to play a major part in chondrocyte proliferation. In light of all of the aforementioned studies, chondrocyte protein receptors present as a possible trigger for pharmacological targets.
Disclosure
Dr. Gordon Slater is the medical director of Integrant Pty Ltd an orthobiologics company. He is a former director of Albury Day Surgery.
References
- Mobasheri A, Matta C, Uzielienè I, Budd E, Martín-Vasallo P, et al. (2019) The chondrocyte channelome: A narrative review. Joint Bone Spine. 86(1):29-35.
- Jeremiasse B, Matta C, Fellows CR, Boocock DJ, Smith JR, et al. (2020) Alterations in the chondrocyte surfaceome in response to pro-inflammatory cytokines. BMC Mol Cell Biol. 21:4.
- Gautam N, Downes GB, Yan K, Kisselev O. (1998) The G-protein betagamma complex. Cell Signal. 10(7):447-55.
- Wu M, Deng L, Zhu G, Li YP. (2010) G Protein and its signaling pathway in bone development and disease. Front Biosci (Landmark Ed.). 15:957-85.
- Keinan D. (2014) Role of regulator of G protein signaling proteins in bone. Front Biosci. (Landmark Ed.)19:634-48.
- Sakamoto A, Chen M, Kobayashi T, Kronenberg HM, Weinstein LS. (2005) Chondrocyte-specific knockout of the G protein G(s)alpha leads to epiphyseal and growth plate abnormalities and ectopic chondrocyte formation. J Bone Miner Res. 20(4):663-71.
- Chagin AS, Vuppalapati KK, Kobayashi T, Guo J, Hirai T, et al. (2014) G-protein stimulatory subunit alpha and Gq/11alpha G-proteins are both required to maintain quiescent stem-like chondrocytes. Nat Commun. 5:3673.
- Klemke M, Pasolli HA, Kehlenbach RH, Offermanns S, Schultz G, et al. (2000) Characterization of the extra-large G protein alpha-subunit XLalphas. II. Signal transduction properties. J Biol Chem. 275(43):33633-40.
- Jikko A, Murakami H, Yan W, Nakashima K, Ohya Y, et al. (1996) Effects of cyclic adenosine 3',5'-monophosphate on chondrocyte terminal differentiation and cartilage-matrix calcification. Endocrinology. 137(1):122–8.
- Lee K, Deeds JD, Bond AT, Juppner H, Abou-Samra AB, et al. (1993) In situ localization of PTH/PTHrP receptor mRNA in the bone of fetal and young rats. Bone. 14(3):341–345.
- Clark CA, Schwarz EM, Zhang X, Ziran NM, Drissi H, et al. (2005) Differential regulation of EP receptor isoforms during chondrogenesis and chondrocyte maturation. Biochem Biophys Res Commun. 328(3):764–76.
- de Brum-Fernandes AJ, Morisset S, Bkaily G, Patry C. (1996) Characterization of the PGE2 receptor subtype in bovine chondrocytes in culture. Br J Pharmacol. 118(7):1597–1604.
- Jones SW, Brockbank SMV, Mobbs ML, Le Good LJ, Soma-Haddrick S, et al. (2006) The orphan G-protein coupled receptor RDC1: evidence for a role in chondrocyte hypertrophy and articular cartilage matrix turnover. Osteoarthritis Cartilage. 14(6):597-608.
- Hoebertz A, Townsend-Nicholson A, Glass R, Burnstock G, Arnett TR. (2000) Expression of P2 receptors in bone and cultured bone cells. Bone. 27(4):503–510.
- Kaplan AD, Kilkenny DM, Hill DJ, Dixon SJ. (1996) Extracellular nucleotides act through P2U purinoceptors to elevate [Ca2+] and enhance basic fibroblast growth factor-induced proliferation in sheep chondrocytes. Endocrinology. 137(11):4757–766.
- Lai LP, Mitchell J. (2008) Beta2-adrenergic receptors expressed on murine chondrocytes stimulate cellular growth and inhibit the expression of Indian hedgehog and collagen type X. J Cell Biochem. 104(2):545-53.
- Fukuda K, Matsumura F, Tanaka S. (1993) Histamine H2 receptor mediates keratansulfate secretion in rabbit chondrocytes: role of cAMP. Am J Physiol. 265:C1653-C1657.
- Nurminsky D, Magee C, Faverman L, Nurminskaya M. (2007) Regulation of chondrocyte differentiation by actin-severing protein adseverin. Dev Biol. 302(2):427-437.
- Chagin AS, Kronenberg HM. (2014) G-proteins in differentiation of epiphyseal chondrocytes. J Mol Endocrinol. 53(2):R39-R45.
- Wang G, Woods A, Agoston H, Ulici V, Glogauer M, et al. (2007) Genetic ablation of Rac1 in cartilage results in chondrodysplasia. Dev Biol. 306(2):612-23
- Borzi RM, Mazzetti I, Cattini L, Uguccioni M, Baggiolini M, et al. (2000) Human chondrocytes express functional chemokine receptors and release matrix-degrading enzymes in response to C-XC and C-C chemokines. Arthritis Rheum. 43(8):1734-41.
- Neves SR, Ram PT, Iyengar R. (2002) G protein pathways. Science. 296(5573):1636-39
- Chubinskaya S, Hakimiyan A, Pacione C, Yanke A, Rappoport L,et al. (2007) Synergistic effect of IGF-1 and OP-1 on matrix formation by normal and OA chondrocytes cultured in alginate beads. Osteoarthritis Cartilage. 15(4):421-30.
- Bluteau G, Conrozier T, Mathieu P, Vignon E, Herbage D, et al. (2001) Matrix metalloproteinase-1, -3, -13 and aggrecanase-1 and -2 are differentially expressed in experimental osteoarthritis. Biochim Biophys Acta. 1526:147-58.
- Mitchell PG, Magna HA, Reeves LM, Lopresti Morrow LL, Yocum SA, et al. (1996) Cloning, expression, and type II collagenolytic activity of matrix metalloproteinase-13 from human osteoarthritic cartilage. J Clin Invest. 97:761e8.
- Sylvia VL, Del Toro F Jr, Hardin RR, Dean DD, Boyan BD, et al. (2001) Characterization of PGE(2) receptors (EP) and their role as mediators of 1alpha,25-(OH)(2)D(3) effects on growth zone chondrocytes. J Steroid Biochem Mol Biol 78(3):261-74.
- DelToroJr, Sylvia VL, Schubkegel SR, Campos R, Dean DD, et al. (2000) Characterization of prostaglandin E(2) receptors and their role in 24,25-(OH)(2)D(3)-mediated effects on resting zone chondrocytes. J Cell Physiol. 182(2):196-208.
- Harris SG, Padilla J, Koumas L, Ray D, Phipps RP. (2002) Prostaglandins as modulators of immunity. Trends Immunol. 23(3):144-50.
- Fedyk ER, Phipps RP. (1996) Prostaglandin E2 receptors of the EP2 and EP4 subtypes regulate activation and differentiation of mouse B lymphocytes to IgE-secreting cells. Proc Natl Acad Sci. USA. 93(20):10978-983.
- Zhang X, Schwarz EM, Young DA, Puzas JE, Rosier RN, et al. (2002) Cyclooxygenase-2 regulates mesenchymal cell differentiation into the osteoblast lineage and is critically involved in bone repair. J Clin Invest. 109(11):1405–1415.
- Simon AM, Manigrasso MB, OConnor JP. (2002) Cyclo-oxygenase 2 function is essential for bone fracture healing. J Bone Miner Res. 17(6):963-76.
- Caswell AM, Leong WS, Russell RG. (1991) Evidence for the presence of P2-purinoreceptors at the surface of human articular chondrocytes in monolayer culture. Biochim Biophys Acta. 1074(1):151-8.
- Kanof PD, Greengard P. (1979) Pharmacological properties of histamine-sensitive adenylcyclase from guinea pig cardiac ventricular muscle. Mol Pharmacol.15(3):445-61.
- Malone DG, Irani AM, Schwartz LB, Barrett KE, Metcalfe DD. (1986) Mast cell numbers and histamine levels in synovial fluids from patients with diverse arthritides. Arthritis Rheum. 29(8): 944-55.
- Chenu C, Serre CM, Raynal C, Burt-Pichat B, Delmas PD. (1998) Glutamate receptors are expressed by bone cells and are involved in bone resorption. Bone 22(4):295-99.
- Gilbert RW, Szczesniak AM, Langman MF, Anderson G I. (1999) Variation in expression of glutamate receptor subunits in skeletal tissue with mechanical loading. J Bone Miner Res. S489-S489.
- Maria S. (2016) Interplay between CaSR and PTH1R signaling in skeletal development and osteoanabolism. Semin Cell Dev Biol. 49:11-23.
- Chang WH, Tu C, Chen TH, Bikle D, Shoback D. (2008) The extracellular calcium-sensing receptor (CaSR) is a critical modulator of skeletal development. Sci Signal. 1(35):ra1.
- Enomoto H, Inoki I, Komiya K, Shiomi T, Ikeda E, et al.(2003) Vascular endothelial growth factor isoforms and their receptors are expressed in human osteoarthritic cartilage. Am J Pathol. 162(1): 171-181.
- Sakibaei M, Schulze-Tanzil G, Mobasheri A, Beichler T, Dressler J, et al. (2003) Expression of the VEGF receptor-3 in osteoarthritic chondrocytes: stimulation by interleukin-1 beta and association with beta 1-integrins. Histochem Cell Biol. 120(3):235-41.
- Carlevaro MF, Cermelli S, Cancedda R, DescalziCancedda F. (2000) Vascular endothelial growth factor (VEGF) in cartilage neovascularization and chondrocyte differentiation: auto-paracrine role during endochondral bone formation. J Cell Sci.113:59-69.
- Von der Mark K, Gauss V, Von der Mark H, Muller P. (1977) Relationship between cell shape and type of collagen synthesised as chondrocytes lose their cartilage phenotype in culture. Nature. 267(5611):531-32.
- Enomoto-Iwamoto M, Iwamoto M, Nakashima K, Mukudai Y, Boettiger D, et al. (1977) Bone Miner. Inflammation, Lifestyle and Chronic Diseases. Res. 1124–1132.
- Vuori K, Ruoslahti E. (1944) Association of insulin receptor substrate-1 with integrins. Science. 266(5190):1576-8.
- Trippel SB, Corvol MT, Dumontier MF, Rappaport R, Hung HH, et al. (1989) Effect of somatomedin-C/insulin-like growth factor I and growth hormone on cultured growth plate and articular chondrocytes. Res. 25(1):76-82.
- Loeser RF. (1977) Integrins and chondrocyte–matrix interactions in articular cartilage. Arthr Rheum. Matrix Biol. 39:11-6.
- Shakibaei M, John T, De Souza P, Rahmanzadeh R , Merker HJ. (1999) Signal transduction by β1 integrin receptors in human chondrocytes in vitro: collaboration with the insulin-like growth factor-I receptor. Biochem J. 342:615-23.
- Camper L. (1998) Isolation, cloning, and sequence analysis of the integrin subunit alpha10, a beta1-associated collagen binding integrin expressed on chondrocytes. J Biol Chem. 273(32):20383-9.
- Durr J. (1996) Identification and immunolocalization of laminin in cartilage. Exp Cell Res. 22(1):225-33.
- Dürr J, Goodman S, A Potocnik, H von der Mark, K von der Mark. (1993) Localization of beta 1-integrins in human cartilage and their role in chondrocyte adhesion to collagen and fibronectin. Exp Cell Res. 207(2):235-44.
- RF Loeser, CS Carlson, MP McGee. (1995) Expression of beta 1 integrins by cultured articular chondrocytes and in osteoarthritic cartilage. Exp Cell Res. 217(2):248-57.
- Salter DM. (1992) Integrin expression by human articular chondrocytes. Br J Rheumatol. 31(4): 231-34.
- Woods VL Jr. (1994) Integrin expression by human articular chondrocytes, Arthritis Rheum. 37:537-44.
- Holmvall K, Camper L, Johansson S, Kimura JH, Lundgren-Akerlund E. (1995) Chondrocyte and chondrosarcoma cell integrins with affinity for collagen type II and their response to mechanical stress. Exp Cell Res. 221(2):496-503.
- Salter DM, Godolphin JL, Gourlay MS. (1995) Chondrocyte heterogeneity: immunohistologically defined variation of integrin expression at different sites in human fetal knees. J Histochem Cytochem. 43(4):447-57.
- Loeser RF. (2000) Integrin expression by primary and immortalized human chondrocytes: evidence of a differential role for alpha1beta1 and alpha2beta1 integrins in mediating chondrocyte adhesion to types II and VI collagen. Osteoarthritis Cartilage. 8(2):96-105.
- Makihira S. (1999) Enhancement of cell adhesion and spreading by a cartilage-specific noncollagenous protein, cartilage matrix protein (CMP/Matrilin-1), via integrin alpha1beta1. J Biol Chem. 274(16):11417-11423.
- Sillat T, Barreto G, Clarijs P, Soininen A, Ainola M, et al. (2013) Toll-like receptors in human chondrocytes and osteoarthritic cartilage. Acta Orthopaedica. 84(6):585-92.
- Bobacz K, Erlacher L, Smolen J, Soleiman A, Graninger WB.(2004) Chondrocyte number and proteoglycan synthesis in the aging and osteoarthritic human articular cartilage. Ann Rheum Dis. 63:1618-22.
- Usami Y, Gunawardena AT, Iwamoto M, Enomoto-Iwamoto M. (2016) Wnt signaling in cartilage development and diseases: lessons from animal studies. Lab Invest. 96(2):186-96.
- Chun JS, Oh H, Yang S, Park M. (2008) Wnt signaling in cartilage development and degeneration. BMB Rep.41:485-94.
- Nordberg RC, Mellor LF, Krause AR, Donahue HJ, Loboa EG. (2019) LRP receptors in chondrocytes are modulated by simulated microgravity and cyclic hydrostatic pressure. PLoS One. 14(10): e0223245.
- Papathanasiou I, Malizos KN, Tsezou A. (2010) Low-density lipoprotein receptor-related protein 5 (LRP5) expression in human osteoarthritic chondrocytes. J Orthop Res. 28(3):348-53.
- Joiner DM, Less KD, Van Wieren EM, Hess D, Williams BO. (2013) Heterozygosity for an inactivating mutation in low-density lipoprotein-related receptor 6 (Lrp6) increases osteoarthritis severity in mice after ligament and meniscus injury. Osteoarthritis Cartilage. 21(10):1576-85.
- Giovannini S, Diaz-Romero J, Aigner T, Mainil-Varlet P,Nesic D. (2010) Population doublings and percentage of S100-positive cells as predictors of in vitro chondrogenicity of expanded human articular chondrocytes. J Cell Physiol. 222:411-20.
- Jones JI, Clemmons DR. (1995) Insulin-like growth factors and their binding proteins: Biological actions. Endocr Rev.16(1):3-34.
- Giannoni P, Cancedda R. (2006) Articular chondrocyte culturing for cell-based cartilage repair: Needs and perspectives. Cells Tissues Organs. 184(1):1-15.
- Bhardwaj N, Devi D, Mandal BB. (2015) Tissue-engineered cartilage: The crossroads of biomaterials, cells and stimulating factors. Macromol Biosci. 15:153-182.
- Shi Y, Massagué J. (2003) Mechanisms of TGF-beta signaling from cell membrane to the nucleus. Cell. 113:685-700.
- Witt A, Salamon A, Boy D, Hansmann D, Büttner A, et al. (2017) Gene expression analysis of growth factor receptors in human chondrocytes in monolayer and 3D pellet cultures. Int J Mol Med. 40(1):10-20.
- Pulai JI, Chen H, Im HJ, Kumar S, Hanning C, Hegde PS, et al. (2005) NF-kappa B mediates the stimulation of cytokine and chemokine expression by human articular chondrocytes in response to fibronectin fragments. Immunol. 174(9):5781-8.
- Alaaeddine N, Olee T, Hashimoto S, Creighton-Achermann L, Lotz M. (2001) Production of the chemokine RANTES by articular chondrocytes and role in cartilage degradation. Arthritis Rheum. 44(7):1633-43.
- Cuellar JM, Scuderi GJ, Cuellar VG, Golish SR, Yeomans DC. (2009) Diagnostic utility of cytokine biomarkers in the evaluation of acute knee pain. J Bone Joint Surg Am. 91(10):2313-20.
- Scanzello CR, McKeon B, Swaim BH, DiCarlo E, Asomugha EU, et al. (2011) Synovial inflammation in patients undergoing arthroscopic meniscectomy: molecular characterization and relationship to symptoms. Arthritis Rheum. 63(2):391-400.
- Pickens SR, Chamberlain ND, Volin MV, Pope RM, Mandelin AM, et al. (2011) Characterization of CCL19 and CCL21 in rheumatoid arthritis. Arthritis Rheum.63(4):914-22.
- Yang MH, Wu FX, Xie CM, Qing YF, Wang GRet al. (2009) Expression of CC chemokine ligand 5 in patients with rheumatoid arthritis and its correlation with disease activity and medication. Chin Med Sci J. 24(1):50-4.
- KoolpeM, Pearson D, and Benton HP. (1999) Expression of both P1 and P2 purine receptor genes by human articular chondrocytes and profile of ligandmediated prostaglandin E2 release. Arthritis Rheum. 42:258-67.
- Loeser RF. (2002) Integrins and cell signaling in chondrocytes. Biorheology. 39(1-2):119-24.
- Shakibaei M, John T, De Souza P,Rahmanzadeh R, Merker HJ. (1999) Signal transduction by β1 integrin receptors in human chondrocytes in vitro: collaboration with the insulin-like growth factor-I receptor. Biochem J.342(3):615-23.

