Mesenchymal Stem Cell-Derived Exosome Treatment for Acne Scars: An Alternative Therapy
Silvina Pastrana-López*
M.D. Márquez-Lomas, Andrea (Medical Researcher) Cellular Hope Institute, Cancún. México
*Corresponding author: Silvina Pastrana-López, M.D. Márquez-Lomas, Andrea (Medical Researcher) Cellular Hope Institute, Cancún. México
Citation: Pastrana-Lopez S. (2024) Mesenchymal Stem Cell-Derived Exosome Treatment for Acne Scars: An Alternative Therapy. J Stem Cell Res. 5(2):1-15.
Received: June 10, 2024 | Published: June 26, 2024
Copyright© 2024 genesis pub by Pastrana-Lopez S. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation
DOI: https://doi.org/10.52793/JSCR.2024.5(2)-S2(2)
Abstract
Acne vulgaris and acne scars are inflammatory dermatological issues that can affect both adolescents and adults, manifesting with varying characteristics across populations. The exact prevalence of acne vulgaris and acne scars is uncertain, but it is estimated to significantly impact young adults. In adults, patients with acne vulgaris can develop permanent scars, which not only have an aesthetic impact but can also negatively affect mental health and quality of life. The clinical manifestations of acne vulgaris can include open or closed comedones, papules, pustules, nodules, cysts, erythema, and/or seborrhea, which can mature into ice-pick, rolling, boxcar, hypertrophic, keloid scars, or hyperpigmentation. Early diagnosis of acne vulgaris is crucial to prevent dermatological damage and improve long-term prognosis. Severe cases of inflammatory acne have a higher likelihood of resulting in scarring. Management of acne scars focuses on topical treatments such as retinoids; therapies like microneedling, lasers, subcision, dermal fillers, deep chemical peels; and biological and regenerative therapies such as Platelet-Rich Plasma (PRP) or mesenchymal stem cell-derived exosomes (MSC). Recent adv0061nces in regenerative medicine have introduced MSC-derived exosomes as a promising treatment. This article details the clinical case of a 33- year-old female patient with severe acne scars treated with MSC-derived exosomes, highlighting the treatment process, results, and implications for future therapeutic strategies
Introduction
A significant proportion of the population is affected by acne scars, which frequently lead to psychological and social difficulties. Acne vulgaris is one of the most common dermatological conditions, affecting around 85% of adolescents and a significant proportion of young adults. The prevalence of acne scars varies widely, with approximately 20-30% of those who have had acne experiencing permanent skin sequelae. Although conventional treatments such as laser therapy, microneedling, and chemical peels may achieve some degree of success, they often fail to completely eliminate deep scars. Mesenchymal stem cell-derived exosomes, with their regenerative and anti- inflammatory capabilities, offer a novel perspective in scar treatment. This case study examines the effectiveness of this treatment in a patient with long-lasting acne scars.
Epidemiology and Ethiology
Acne vulgaris can affect individuals of any age, including adults. However, it tends to be more prevalent among adolescents, with 30-95% experiencing acne at some point. Of these, it is estimated that around 20% will develop clinically significant acne scars. In adults, between 1% and 12% continue to suffer from active acne, and of these, approximately 14% will develop scars. The etiopathogenesis can be highly variable, considering various inflammatory, collagen production, genetic, manipulation, or infectious factors. Inflammatory factors where inflammatory mediators such as cytokines and enzymes (e.g., matrix metalloproteinases) break down extracellular matrix components contribute to scar formation [1]. The lack of collagen production causes the skin tissue to be unable to produce enough new collagen to replace damaged tissue, resulting in depressed scars [2]. Overproduction of collagen, where the body produces too much collagen during the healing process, results in raised and often discolored scars. Factors such as skin type, sun exposure, and general skin care can influence scar formation. UV radiation can worsen scar appearance by causing hyperpigmentation and further skin damage. Mechanical manipulation such as picking, squeezing, or attempting to pop acne lesions can exacerbate inflammation and increase the likelihood of scarring. This physical trauma can disrupt the normal healing process and lead to more pronounced scars [1]. Secondary bacterial infections can aggravate acne lesions, increasing inflammation and tissue damage, prolonging the healing process, and increasing scarring.
Clinical Characteristics
Acne scars are permanent sequelae of inflammatory acne lesions and can be similar in both adolescents and adults. They exhibit different morphologies and clinical characteristics, which can be mainly divided into atrophic scars, hypertrophic scars, and keloids.
Atrophic scars
- Ice-pick or "V" scars: Represent 60%-70% of total scars. These are narrow, deep, and punctate scars with sharp edges extending deep into the dermis. Commonly found on the cheeks and other areas with thicker skin [3] (Figure 1.C).
- "U" or boxcar scars: Broad, round or oval depressed scars with well-defined edges. They can be superficial (0.1 to 0.5 mm) or deeper (greater than 0.5 mm). Frequently found on the cheeks and jawline [4] (Figure 1.B).
- Rolling scars: Superficial, wavy scars giving the skin an uneven appearance, generally larger than 4 to 5 mm. Typically appear in areas with thicker skin like the cheeks [5] (Figure 1A).
Hypertrophic scars and keloids
- Hypertrophic scars: Elevated, firm scars that remain within the original lesion's boundaries. Often develop in high-tension areas of the skin, such as the jaw and back. They may initially appear red or purple and become paler over time [6] (Figure 1.D).
- Keloids: Elevated, thick scars that extend beyond the original lesion's boundaries and can continue to grow over time. Commonly found on the chest, shoulders, back, and jawline. They can be red, purple, or hyperpigmented.
Figure 1: Tipos de cicatrices por acné
Post-inflammatory hyperpigmentation
Dark spots: Varying from light to dark brown, depending on the individual's skin tone, persisting after acne lesions have healed. These are not true scars but can be persistent and distressing for patients [7].
Diagnosis
The diagnosis of acne scars is made through clinical evaluation, observation of scars, and using acne scar scales. Below is an overview of the steps and criteria for the observation and classification of acne scars:
- Clinical Evaluation: The diagnostic process begins with a thorough clinical inspection by an experienced physician or dermatologist. This includes reviewing the patient's acne history, previous treatments, and their response to these treatments.
- Physical Examination: Visual inspection and palpation of the scars to determine type, severity, and depth.
- Medical Photography: Documenting the scars photographically to compare progress before and after treatment.
Evaluation scales
Acne Scar Assessment Scale (ECCA): This scale aims to classify the severity of scars based on type and extent for treatment purposes. It is divided into two scoring sections, specific types giving points for different scar types, and semi- quantitative evaluation, which scores based on the extent and number of scars. The total score can range from 0 to 540. The advantages of this system include accounting for all scar types [8] (Table 1).
|
DESCRIPTION |
(A) |
ESCALE (B) |
AXB |
|
Ice pick atrophic scars (V) Diameter < 2 mm Punctiform |
15 |
0 = No scar 1 = Few scars 2 = Limited number of scars 3 = Many scars |
|
|
Rectangular atrophic scars (U) Diameter 2-4 mm, with edges sloping inward |
20 |
0 = No scar 1 = Few scars 2 = Limited number of scars 3 = Many scars |
|
|
Rolling atrophic scars (M) Diameter > 4 mm, with edges sloping inward |
25 |
0 = No scar 1 = Few scars 2 = Limited number of scars 3 = Many scars |
|
|
Superficial elastosis |
30 |
0 = No scar 1 = Few scars 2 = Limited number of scars 3 = Many scars |
|
|
Pre-score 1: |
|||
|
Hypertrophic and inflammatory scars, less than two years old |
40 |
0 = No scar 1 = Few scars 2 = Limited number of scars 3 = Many scars |
|
|
Keloid scars Hypertrophic scars, more than two years old |
50 |
0 = No scar 1 = Few scars 2 = Limited number of scars 3 = Many scars |
|
|
Total Score: |
|
|
|
Table 1: Acne Scar Clinical Evaluation Scale (ECCA).
Patient and Observer Scar Assessment Scale (POSAS): Combines patient and physician evaluations to provide a more comprehensive assessment. It consists of 6 categories (vascularity, pigmentation, relief, roughness, flexibility, surface area). These categories are rated on a scale of 1 (similar to normal skin) to 10 (very different from normal skin). The sum of the 6 categories results in the total score [9] (Table 2).
1=Similar to the skin 10=Very different from the skin.
|
Parameter |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
1 0 |
Category |
|
Vascularity |
|
|
|
|
|
|
|
|
|
|
Pale/Pink/Red/Purple / Mixed |
|
Pigmentatio n |
|
|
|
|
|
|
|
|
|
|
Hypo/Hyper/Mixed |
|
Elevation |
|
|
|
|
|
|
|
|
|
|
Thick/Thinned |
|
Roughness |
|
|
|
|
|
|
|
|
|
|
More/Less/Mixed |
|
Flexibility |
|
|
|
|
|
|
|
|
|
|
Flexible/Stiff/Mixed |
|
Surface area |
|
|
|
|
|
|
|
|
|
|
Expansion/Retraction / Mixed |
|
Overall opinion |
|
|
|
|
|
|
|
|
|
|
|
Table 2. Patient and Observer Scar Assessment Scale (POSAS).
Treatment
The goal of acne scar treatment is to reduce the appearance of scars and smooth the skin. Below is a summary of treatment options:
Topical treatments
- Topical Retinoids: Can improve skin texture and reduce the appearance of superficial scars.
- Silicone Gel or Patch: Used to improve the appearance of hypertrophic scars and keloids.
Procedural treatments
- Microneedling: Uses fine needles to create small punctures in the skin, stimulating collagen and elastin production, thus promoting mechanical abrasion over damaged areas. The penetration is superficial, removing the outer layer of the dermis and accelerating the natural exfoliation process.
- Laser Therapy (Fractional CO2 Laser, Erbium Laser): Removes superficial skin layers and stimulates collagen production, improving texture and reducing scar depth. The choice of laser type should consider the nature of the scar, patient tolerance, and expectations. Patients with boxcar scars are the best candidates [10].
- Sub Cision: A procedure where a Nokor needle is inserted under the skin adjacent to the scar with the bevel up on the deep dermis. Fan-like movements are performed to break the fibrous bands causing the rolling scars. Improvement is observed 6 months post- treatment [11].
- Dermal Fillers (Hyaluronic Acid): Used to elevate depressed scars, providing a more even skin surface. Effective for boxcar scars but not for ice-pick scars [12].
- High-Power Chemical Peels: Apply strong acids to remove superficial skin layers and promote regeneration. More effective on macular scars compared to deeper ice-pick and rolling scars, which require periodic sequential peels for better results [13].
Biological and regenerative treatments
- Platelet-Rich Plasma (PRP): A mixture of high-concentration platelets with growth factors, obtained by one-phase centrifugation of blood tissue. It contains large amounts of proteins like platelet-derived growth factor, beta fraction growth factor, epithelial growth factor, and adhesion molecules. Injected into the skin to promote cellular regeneration and collagen production [14].
- Mesenchymal Stem Cell-Derived Exosomes: Contain growth factors and bioactive molecules that promote skin repair and regeneration, significantly improving acne scars.
- Treating acne scars involves a multifaceted approach, and the choice of treatment should be tailored to the scar type, skin type, and specific patient preferences. A combination of multiple treatments often yields the best results.
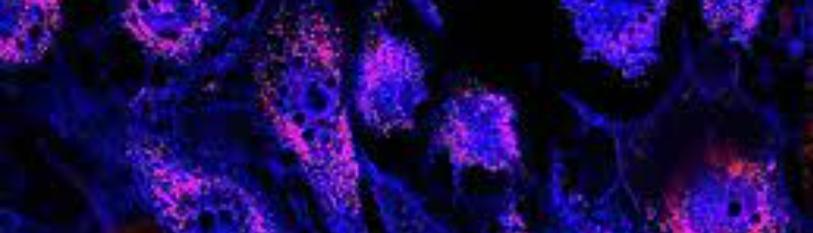
Exosomes
Exosomes are extracellular nanovesicles, typically between 30-200 nanometers in diameter, released by cells as a means of communication, tissue repair, and immunomodulation (Figure 2.A). These nanovesicles contain a significant amount of lipids, proteins, and genetic material such as mRNA and miRNA. Additionally, exosomes possess anti-inflammatory and immunomodulatory properties, making them ideal for addressing facial laxity (Figure 2.B).
Recently, exosomes have gained prominence in the cosmetic world. Studies have shown that exosomes are beneficial for skincare due to their high content of proteins, lipids, and other molecules that can promote healing, hydration, and skin protection. These molecules have the potential to stimulate collagen production, reduce inflammation, and protect the skin against the negative effects of the environment. Exosomes also have the ability to reduce reactive oxygen species (ROS) and TNF-α while increasing TGF- β, leading to an increase in MMP-1 and type I procollagen [15].
Moreover, cytokines, nucleic acids, proteins, and other bioactive substances present in exosomes can help protect the skin from harmful environmental factors and reduce dark spots and discoloration. Exosome therapy can be applied topically or injected directly into scar tissue. Injections are often used to treat deeper scars due to their effective penetration into the dermis where the scar tissue resides. Topical applications may be more suitable for treating superficial scars, as they allow for a more uniform distribution of therapeutic agents. Clinical studies have confirmed that exosome therapy is safe and effective for scar removal. It has the potential to reduce the appearance of skin marks, increase skin hydration and elasticity, and decrease inflammation. Additionally, it can help strengthen the skin's natural defenses against infections.
Exosomes derived from umbilical cord mesenchymal stem cells (UCMSC) have an increased concentration of certain microRNAs, such as miR-21, miR-23a, miR-125b, and miR- 145 [16]. Furthermore, exosomes rich in miR-21-3p were found to promote epithelial regeneration, reduce scar size, and stimulate the formation of new blood vessels by inhibiting PTEN and SPRY1 [17].
Accordingly, it can be inferred that exosomes derived from mesenchymal stem cells (MSCs), including ADSC-exos, could regulate fibroblast function and collagen production to promote scar- free healing. Therefore, exosomes derived from umbilical cord mesenchymal stem cells could be a viable therapeutic option for promoting wound healing, preventing scar formation and reducing scar appearance.
Figure 2 (A): Schematic Representation of Exosome Biogenesis and Secretion
Figure 2 (B): Molecular Components of Exosomes (Tenchov 2022).
Case Report
A 33-year-old female patient with no relevant medical history experienced recurrent nodules and papules of acne vulgaris on her face during adolescence. Initial treatment included facial cleanings and laser sessions without the need for antibiotics. To maintain the treatment, weekly facial cleanings were conducted along with the use of topical medications, which temporarily controlled the condition.
Subsequently, at the age of 24, the patient developed nodular cystic acne, a more severe form of the condition, which persisted for two to three years. During this period, she was administered isotretinoin at a dose of 20 mg per day for eight months on three different occasions. The patient noted that during this period, she did not use facial moisturizers or UV sunblock and engaged in self-manipulation of the acne. Nevertheless, she continued with biweekly facial cleanings and the use of antiseborrheic soap.
At the age of 30, the patient observed an improvement in her acne condition. However, she began to develop residual ice pick scars, boxcar scars, rolling scars, and hyperpigmentation (Figure 3). To address these scars, she underwent several aesthetic procedures. Initially, three sessions of glycolic acid chemical peels were performed, significantly improving skin hyperpigmentation. Subsequently, four sessions of CO2 laser treatment were applied, resulting in a notable improvement in ice pick scars. To complement these treatments, the patient incorporated subcision treatments and topical treatments, which included the use of sunscreen, morning vitamin C, moisturizer both in the morning and at night, topical and oral retinol (soluble vitamin A), and three applications of collagenase.
Figure 3: Patient Admission with Ice Pick, Boxcar, and Rolling Scars. (A) Right Hemisphere (B) Right Hemisphere (C) Left Hemisphere
Additionally, advanced therapies such as the use of Skin Booster and PRP were implemented, with continuous deep cleanings once a month. The patient also began supplementing with megadoses of vitamin C, observing a significant disappearance of acne along with a drastic change in diet. Furthermore, hyaluronic acid filler was applied directly to the scars in three sessions, with a frequency of once every four months.
The patient presented to the clinic with boxcar scars, rolling scars, ice pick scars, and hyperpigmentation, scoring 180 points on the Acne Scar Clinical Evaluation Scale (ECCA). After the examination, pre-treatment photos were taken for case follow-up. The patient's treatment plan included two sessions of subcision and Flow exosome treatment, followed by two sessions of PRP applied with microneedling, with a 45-60 day interval between each treatment.
Figure 4: Control photos at the beginning of the treatment showing ice pick scars, rolling scars, boxcar scars, and hyperpigmentation. Scoring 180 on the ECCA scale (A) Right hemisphere (B) Left hemisphere.
The treatment was applied using subcision with a Nokor needle and exosome infiltration with a 25g cannula in a radiated manner in the deep dermal plane to stimulate extracellular matrix production, reduce fibrosis, and decrease inflammation. Flow exosomes from the Cellgenic brand were used, containing 30 billion exosomes derived from umbilical cord mesenchymal stem cells from Wharton's jelly. These exosomes contain trace elements, amino acids, interleukins, vitamins, growth factors, and proteins (Table 3-5).
|
Components |
Molecular weight |
Concentration mg/L |
|
Amino acids |
75 |
10 |
|
L-arginine |
174 |
200 |
|
L-asparagine |
132 |
50 |
|
L-apartic acid |
133 |
20 |
|
L-cysteine 2HCl |
313 |
65 |
|
L-glutamic acid |
147 |
20 |
|
L-glutamine |
146 |
300 |
|
L-histidine |
155 |
15 |
|
L- hydroxyproline |
131 |
20 |
|
L-isoleucine |
131 |
50 |
|
L-leucine |
131 |
50 |
|
L-lysine hydrochloride |
183 |
40 |
|
L-methionine |
149 |
15 |
|
L- phenylalanine |
165 |
15 |
|
L-proline |
115 |
20 |
|
L-serine |
105 |
30 |
|
L-threonine |
119 |
20 |
|
L-tryptophan |
204 |
5 |
|
L-tyrosine adenine phosphate |
261 |
29 |
|
L-valine |
117 |
20 |
Table 3: Amino acids in Flow exosome vial.
|
Factors |
Quantity |
|
Collagen type I and II |
1.643 mg/mL |
|
Hyaluronic acid (HA) |
1.85 ug/mL |
|
Chondroiti n sulfate (CS) |
1.58ug/m L |
|
Stem Cell Factor (SCF) |
38.0 pg/mL |
|
Vascular Endothelial Growth Factor (VEGF) |
1.8 ng/mL |
|
Factors |
Quantity (pg/mL) |
|
GM- CSF |
6.53 |
|
INF- |
2.30 |
|
IL-2 |
8.20 |
|
IL-3 |
1.75 |
|
IL-4 |
9.48 |
|
IL-5 |
0.94 |
|
IL-6 |
633 |
|
IL-7 |
37.0 |
|
IL-8 |
11,278 |
|
IL-10 |
1.40 |
|
IL-18 |
7.70 |
|
MIP-1 |
5.80 |
|
MIP-1 |
18.8 |
|
MCP-1 |
13,714 |
|
TNF- |
6.63 |
|
TNF- |
8.90 |
Table 5: Factors in Flow exosome vial.
Figure 5: After First Treatment with Flow Exosomes, seen a reduction of Ice Pick and Rolling Scars (A) Right Hemisphere (B) Left Hemisphere.
Figure 6: After the second session with Flow exosomes, observing a decrease in rolling, ice pick, and boxcar scars. (A) Left Hemisphere (B) Right Hemisphere.
Figure 7: After the third session with Flow exosomes and PRP, observing a decrease in rolling scars. (A) Right Hemisphere (B) Left Hemisphere and chin.
Figure 8: Fourth and final session with Flow exosomes and PRP, observing total disappearance of ice pick scars. (A) Right Hemisphere.
Figure 8: Fourth and final session with Flow exosomes and PRP, observing total disappearance of ice pick scars. (B) Left Hemisphere.
|
Vitamins |
Molecular weight |
Concentration mg/L |
|
Biotin |
244 |
0.2 |
|
Choline chloride |
140 |
3 |
|
Calcium pantothenate |
477 |
0.25 |
|
Folic acid |
441 |
1 |
|
Niacinamide |
122 |
1 |
|
Para-aminobenzoic acid |
137 |
1 |
|
Pyridoxine hydrochloride |
206 |
1 |
|
Riboflavin |
376 |
0.2 |
|
Thiamine hydrochloride |
337 |
1 |
|
Vitamin B12 |
1355 |
0.005 |
|
Inositol |
180 |
35 |
Table 4: Vitamins in Flow exosome vial.
Results
The patient showed a remarkable evolution in the condition of her skin, from common acne to nodular cystic acne and scarring acne of different types. Multiple management strategies, including dermatological procedures, changes in skincare regimen, and diet, allowed the patient's dermis to appear more uniform. Therapeutic novelties offered, such as exosomes and PRP, which efficiently complement traditional and aesthetic therapies, proved to be highly effective in substantially improving skin tissue and reducing residual marks in the discussed patient. The ECCA score decreased from 180 to 90 points over the course of the sessions, demonstrating a significant improvement in skin appearance.
Conclusion
Subcision with Flow exosomes proved highly effective for severe acne scars. Precise infiltration of exosomes into affected areas led to significant regeneration of scar tissue by promoting collagen formation, improving skin texture, and color. Additionally, angiogenesis promoted by exosomes enhanced skin oxygen supply while also promoting greater nutrition, favoring skin tissue repair and a healthy facial appearance. Furthermore, PRP sessions with microneedling were a beneficial addition to the treatment, contributing to regenerative action and accelerating the healing process. As PRP has regenerative effects, the combination of PRP and exosomes created a favorable environment for skin restoration. The comprehensive treatment of acne and its scars in this patient highlights the need for advanced and individualized approaches. This combination of subcision, exosomes, and PRP was highly effective for the treatment of severe acne scars and resulted in notable improvements in scar regeneration and appearance. In this case, the potential aesthetic benefits of exosomes in dermatology were demonstrated, highlighting their potential as an effective tool for skin regeneration and the treatment of difficult-to-treat scars.
References
-
Lee JY, Yang CC, Chao SC. (2004) Treatment of keloids and hypertrophic scars. Dermat Surg. 30(1):151-54.
-
Jacob CI, Dover JS, Kaminer MS. (2001) Acne scarring: A classification system and review of treatment options. J Am Acad Dermatol. 45(1):109-17.
-
Fabbrocini G, Annunziata MC, D'Arco V, De Vita V, Lodi G, Mauriello MC, Pastore F, Monfrecola G. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract. 2010:893080
-
Tan JK, Tang J, Fung K, Gupta AK, Thomas DR, et al. (2001) Prevalence and severity of facial acne vulgaris in a referral cohort. J Cutan Med Surg. 5(3):177- 80.
-
Goodman GJ, Baron JA. (2006) Postacne scarring: A quantitative global scarring grading system. Dermatol Surg. 5(1):48-52.
-
Saha, A., Sharma, Y. K., & Srivastava, A. (2018). Keloids: Review of etiopathogenesis and management. J Dermatol Treat. 29(6):562-70.
-
Davis EC, Callender VD. (2010) Post inflammatory hyperpigmentation: A review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 3(7):20-31.
-
Dreno B, Khammari A, Orain N, Noray C, Méria`l-Kieny C, et al. (2007) ECCA grading scale: An original validated acne scar grading scale for clinical practice in dermatology. Dermatology. 214(1):46-51.
-
Draaijers LJ, Tempelman FR, Botman YA, Tuinebreijer WE, Middelkoop E, et al. (2004) The patient and observer scar assessment scale: A reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 113(7):1960-65.
-
Sobanko JF, Alster TS. (2012) Management of acne scarring, part I: a comparative review of laser surgical approach. Am J Clin Dermatol. 13(5):319-30.
-
Chandrashekar B, Nandini A. (2010) Acne scar subcision. J Cutan Anesthet Surg. 3(2):125–26.
-
Hasson A, Romero WA. (2010) Treatment of facial atrophic scars with Esthélis, a hyaluronic acid filler with polydense cohesive matrix (CPM). J Drugs Dermatol. 9(12):1507– 09.
-
López Martín Prieto S, Sánchez Conejo Mir J. (2001) Peeling químico con ácido tricloroacético. Un peeling clásico de máxima actualidad. Actas dermo-sifiliogr.(Ed. impr.), 537-547.
-
Cruciani M, Masiello F, Pati I, Pupella S, De Angelis V. (2024) Platelet rich plasma use for treatment of acne scars: an overview of systematic reviews. Blood transfusion. 22(3):226–38.
-
Hu S, Li Z, Cores J, Huang K, Su T, et al. (2019) Needle-free injection of exosomes derived from human dermal fibroblast spheroids ameliorates skin photoaging. ACS nano. 13(10):11273-282.
-
Fang S, Xu C, Zhang Y, Xue C, Yang C, et al. (2016) Umbilical cord- derived mesenchymal stem cell-derived exosomal microRNAs suppress myofibroblast differentiation by inhibiting the transforming growth factor-β/SMAD2 pathway during wound healing. Stem Cells Transl Med. 5(10):1425-39.
-
Hu Y, Rao SS, Wang ZX, Cao J, Tan YJ, et al. (2018) Exosomes from human umbilical cord blood accelerate cutaneous wound healing through miR-21- 3p-mediated promotion of angiogenesis and fibroblast function. Theranostics. 8(1):169-84.
|
This article was originally published in a special issue entitled “Precision Cell Therapy”, handled by Editor Dr. Roni Moya.
|

