IRB Approved Pilot Safety Study of an Extracellular Vesicle Isolate Product Evaluating the Treatment of Osteoarthritis in Combat-Related Injuries
Johnny East DO, Trace Alexander DC, and Maxwell Dordevic,*
Addison Pain & Regenerative Medicine, 16633 Dallas Pkwy Suite 150, USA
*Corresponding author: Maxwell Dordevic, Addison Pain & Regenerative Medicine, 16633 Dallas Pkwy Suite 150, USA
Citation: East DO J, Alexander DC T, Dordevic M. (2020) IRB Approved Pilot Safety Study of an Extracellular Vesicle Isolate Product Evaluating the Treatment of Osteoarthritis in Combat-Related Injuries. 1(2):1-10.
Received: August 15, 2020 | Published: September 25, 2020
Copyright© 2020 genesis pub by Do JE, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License., This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/JSCR.2020.1(2)-09
Abstract
Secreted bone marrow mesenchymal stem cell derived extracellular vesicles (BM-MSC-EVs) are reported to contain hundreds of different growth factors, cytokines, chemokines, micro and messenger RNAs packaged within exosomes. This is the first report on the safety and clinical efficacy of an BM-MSC-EV product (ExoFlo™) to treat osteoarthritis (OA). Thirty-three Navy SEAL veterans were treated with ExoFlo for OA of the knee (n=58), shoulder (n=32), elbow (n=16), hip (n=12), ankle (n=8) or wrist (n=6). At six-month follow-up, the average patient improved 77% in BPI, 80% in ODI, 76% in LEFS, 51% in UEFS, and 77% in QD. All improvements were statistically significant with values of p<0.001. Ninety-five percent of the improvement occurred within the first six weeks following injection. There were no complications or adverse events, minor or major, and no patient was observed to have accelerated OA progression resultant from the ExoFlo injection. These patients will continue to be followed for at least 2-years. At six-month follow-up, a single ExoFlo injection for OA appears safe and clinically efficacious for the treatment of patients with at least grade-2 changes utilizing the Kellgren-Lawrence scale.
Keywords
Regenerative medicine; Osteoarthritis; Extracellular vesicles; xosomes; Growth factors; Bone marrow; Mesenchymal stem cells; Navy SEAL veterans
Abbreviations
Bone Marrow Mesenchymal Stem Cell (BM-MSC), Extracellular Vesicle Isolate Product (EVIP), Extracellular Vesicles (EV), Osteoarthritis (OA), Bone Marrow Concentrate (BMC), Oswestry Disability Index (ODI), Brief Pain Inventory (BPI), Upper Extremity Functional Scale (UEFS), Lower Extremity Functional Scale (LEFS), QuickDASH (QD), Institutional Review Board (IRB), Kellgren-Lawrence scale (K-L scale)
Introduction
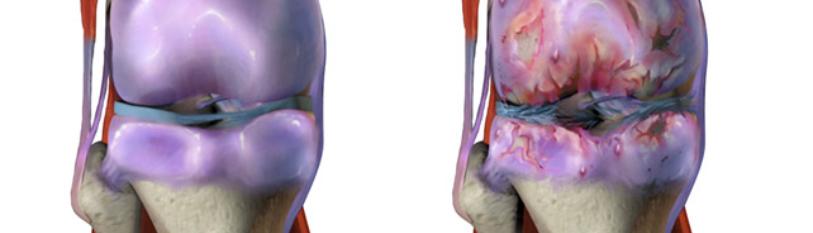
Over 50 million Americans require daily treatment for the disability and pain associated with OA. The surgical treatment for OA is joint arthroplasty and over 1 million total hip and knee replacements are performed every year in the United States, with a direct cost of over $30 billion and an indirect cost of over $200 billion. These numbers are expected to double in the next three years [1,2]. Every day, 10,000 people in the United States turn 65. This demographic trend will continue for the next 14 years (aarp.org), thereby increasing the population of candidates for joint replacements operations. The American Academy of Orthopedic Surgeons (AAOS) recommended treatment for OA of the extremities includes the following: weight loss, gentle exercise, anti-inflammatory medications followed by joint replacement. The AAOS does not recommend arthroscopic debridement or any Hyaluronic Acid (HA) products such as Synvisc®, Euflexxa™, Orthovisc®, Supartz™, or Hyalgan® for treating OA. Four previous prospective randomized studies have shown no benefit over placebo at 6-month follow-up with these HA injections [3-7]. Even though HA products have shown no efficacy, the market for these products is several hundred million dollars per year. The reason for this is the massive void between non-operative treatment options and the surgical treatment for OA, joint arthroplasty. The efficacy of using BM-MSCs for cartilage repair was predicated on the hypothesis that these cells could differentiate into chondrocytes to replace damaged cartilage. However, it is now widely accepted that BM-MSCs efficacy is not due to their direct differentiation into chondrocytes, but instead to secreted factors that promote tissue repair [8-10]. Numerous studies have demonstrated that BM-MSCs secrete Paracrine factors, such as growth factors, cytokines, and extracellular vesicles including exosomes that promote proliferation and matrix synthesis of chondrocytes [11-20].
Among the numerous trophic factors secreted by BM-MSCs, exosomes have been identified as the principal-agent mediating the therapeutic efficacy of MSCs in several disease indications such as myocardial ischemia/reperfusion (I/R) injury, limb ischemia, and pulmonary hypertension [21-23]. Exosomes are small, secreted bi-lipid membrane extracellular vesicles of about 30-150 nm in diameter that are thought to function primarily as paracrine intercellular communication vehicles that transfer bioactive lipids, nucleic acids (mRNAs and microRNAs), and proteins between cells to elicit biological responses in recipient cells [24]. Zhang et al. have reported that human BM-MSC exosomes are efficacious in repairing critical-sized osteochondral defects in rats [25]. They subsequently investigated the mechanism underlying MSC exosome-mediated cartilage repair and published the effects of MSC exosomes on chondrocyte survival, migration, proliferation, matrix synthesis, and macrophage response and associated cytokine production in a rat model. These studies found the MSC exosome treatment to be safe and efficacious [19]. This physician-initiated IRB study's primary objective was to determine first, the safety, and second, the clinical efficacy of intra-articular injection of BM-MSC-derived extracellular vesicles (ExoFlo) to treat combat-related OA in Navy SEAL veterans.
Materials and Methods
Study design
This study was a prospective, open-label, non-randomized IRB approved pilot safety study of a single 2mL ExoFlo injection for the treatment of OA of the knee (n=58), shoulder (n=32), elbow (n=16), hip (n=12), ankle (n=8), or wrist (n=6). The treatment was offered free to study participants. The study protocol for the treatment was approved by an IRB (Institute of Regenerative and Cellular Medicine, Protocol number: APRM-OA-001, IRB approval number: IRCM-2019-226). All patients were counseled and consented as per established IRB requirements. Thirty-three (33) Navy SEAL veterans were enrolled in this study. The study was performed at a single center. The study design details, patient demographics, description of the treatment, injection procedure, and statistical tests performed are described.
All patients were Navy SEAL veterans with a primary complaint consistent with combat-related injuries resulting in moderate to severe knee, shoulder, elbow, hip, ankle, or wrist OA. The United States Navy Sea, Air, and Land (SEAL) Teams, commonly known as Navy SEALs, are a component of the Naval Special Warfare Command and the Navy's primary special operations force. Inclusion criteria required patients to have at least grade-2 changes utilizing the Kellgren-Lawrence scale for OA [26]. Every patient had four joints injected (n=132). Patients underwent a pre-injection medical history and physical examination of all their OA joints. Every Navy SEAL was also evaluated with a Brief Pain Inventory (BPI), Oswestry Disability Index (ODI), Lower Extremity Functional Scale (LEFS), Upper Extremity Functional Scale (UEFS), and a QuickDash Scale (QD). Follow up evaluations were obtained at 12 hours, 24 hours, 48 hours, 2 weeks, 6 weeks, 3 months, and 6 months.
OA was defined by pain and stiffness in the joint, worsened by exercise, and decreased range of motion. Patients treated for OA had radiographs of the joint to rate them 2, 3, or 4 on the Kellgren-Lawrence scale (K-L scale) [26].
Therapeutic description
ExoFlo (Direct Biologics, Austin, TX) is composed of secreted extracellular vesicles, primarily exosomes
and growth factors obtained from bone marrow mesenchymal stem/stromal cells. A CLIA licensed laboratory performed the donor bone marrow screening and testing for the presence of any virus or infective agents. The BM-MSCs have been fully characterized as CD90+, CD166+, CD45- MSCs, and have a master file recorded with the FDA. ExoFlo contains hundreds of different molecular communication molecules (proteins and RNA) within the more than 30 billion extracellular vesicles per milliliter. ExoFlo sterilization is achieved through 0.2µm ultrafiltration, not radiation, using cGMP manufacturing methods to ensure the highest possible safety profile. The product is stored frozen (-80°C) to ensure bioactive stability. It is thawed to room temperature prior to use. As part of the lot release criteria, ExoFlo is evaluated for the presence of specific growth factors, extracellular vesicle concentration, exosome concentration sterility, and particle size distribution to verify that every lot meets product specifications.
Patient demographics
The number of patients undergoing treatment for knee, shoulder, elbow, hip, ankle, and wrist along with average BMI and the average age is shown in Table 1.
|
|
Average |
Range |
|
BMI |
28.5 years |
23-35 |
|
Age (n=33) |
48.8 years |
36-70 |
|
Joints Treated (n=132) |
Knee=58, Shoulder=32, Elbow=16, Hips=12, Ankles=8, Wrist=6 |
|
Table 1: Description of Patient Demographics.
Radiographic Analysis: Every patient underwent a standing AP and lateral radiograph of all OA lower extremity joints and a non-weight bearing AP and lateral radiograph of all OA upper extremity joints just prior to the treatment. Of the 58 knees injected there were 44 K-L 2, 12 K-L 3 and 2 K-L 4 joints. Of the 32 shoulders there were 29 K-L 2 and 3 K-L 3 joints. The 16 elbows had 14 K-L 2 and 2 K-L 3 joints. The 12 hips had 9 K-L 2 and 3 K-L 3 joints. The 8 ankles had 5 K-L 2 and 3 K-L 3 joints (Table 2).
|
|
Knee |
Shoulder |
Elbow |
Hip |
Ankle |
|
K-L 2 |
44 |
29 |
14 |
9 |
5 |
|
K-L 3 |
12 |
3 |
2 |
3 |
3 |
|
K-L 4 |
2 |
0 |
0 |
0 |
0 |
|
Total |
58 |
32 |
16 |
12 |
8 |
Table 2: Kellgren-Lawrence description and total number of each joint injected.
Injection Technique: All of the joint injections were performed by the principal investigator utilizing sterile technique with betadine skin prep. Under fluoroscopic guidance, a 22-gauge needle was placed into the arthritic joint and needle position verified. Needle placement was verified under fluoroscopic control. At this point, 2mL of thawed ExoFlo was placed into the joint. The entire procedure of injecting a maximum of four joints per patient required 30 minutes on average. Patients were not prescribed any pain medications. They were placed on restricted physical activity for 2 weeks following the procedure, which included an immediate passive, low-resistance range of motion was encouraged immediately. After two weeks, patients were allowed to return to full activity.
Statistical Tests
Univariable data comparisons were analyzed by two-tailed Student’s t-test with a 95% confidence interval (α=0.05. Microsoft Excel).
Results
Every patient was evaluated immediately after the injection, and then contacted for follow-up 12 hours, 24 hours, 48 hours, and at 2 weeks, 6 weeks, 3 months, and 6 months to discuss any possible adverse side effects from the ExoFlo injection and to obtain clinical evaluation data. Six-month follow-up data was obtained from all but one Navy Seal (97% follow-up). Adverse events included increased back ache for 24 hrs in one patient, increased joint pain in the injected joint for 24 hours in four patients, a change in bowel habits in one patient for 24 hours, and disturbed sleep for two nights in one patient. No patient was determined to have become clinically worse from the injections. Six months after the ExoFlo administration, the average patient experienced statistically improved outcome measures, as shown in (Figure 1).
The average clinical improvement for each pain and functionality test at each time interval is described in (Table 3). The actual score for each of the five tests at 6 week, 3 months, and 6 month time interval is presented in (Table 4). The overall amount of clinical improvement each patient opined when asked, “How much better does each of your specific joints that were injected feel after 6 weeks and 6 months” is detailed in (Table 5).
Figure 1: Patient progress versus time after EVIP injection into the Knee, Shoulder, Elbow, Hip, Ankle, Wrist (n=132) QD = quickDASH, a measure of function with lower scores being ideal, UEFS= higher number indicates better function, LEFS= Higher scores indicate better function, Brief Pain Inventory (BPI) = higher scores indicate higher pain, ODI =Lower score indicates higher function. All p values were <0.001for all timepoint versus baseline comparisons.
|
|
6 Week |
3 Month |
6 Month |
|
BPI |
68.73% Improvement |
72.15% Improvement |
77.22% Improvement |
|
ODI |
65.62% Improvement |
75.62% Improvement |
80.39% Improvement |
|
UEFS |
39.78% Improvement |
51.01% Improvement |
50.95% Improvement |
|
LEFS |
52.09% Improvement |
68.37% Improvement |
75.60% Improvement |
|
QD |
65.31% Improvement |
73.72% Improvement |
77.24% Improvement |
|
All tests showed functional and pain improvements at six months. Brief Pain Inventory (BPI)= higher scores indicate higher pain; ODI =Lower score indicates higher function; UEFS= higher number indicates better function; LEFS= Higher scores indicate better function; QD = QuickDASH, a measure of function with lower scores being ideal. All values had a p<0.001.
|
|||
Table 3: Percentage Improvement from Baseline at Each Follow-up Interval.
|
|
Baseline |
6 Week |
12 Week |
6 Month |
|
BPI |
48.29 |
15.10 |
13.45 |
11.00 |
|
ODI |
28.71 |
9.87 |
7.00 |
5.63 |
|
UEFS |
49.32 |
68.74 |
74.48 |
74.45 |
|
LEFS |
39.68 |
60.35 |
66.81 |
69.68 |
|
QD |
42.23 |
14.65 |
11.10 |
9.61 |
Table 4: Raw mean Test Scores at Baseline and Each Follow-up Interval.
|
|
LT. KNEE |
RT. Knee |
LT. Shld |
RT. Shld |
LT. Hip |
RT. Hip |
LT. Ankle |
RT. Ankle |
LT. Elbow |
RT. Elbow |
LT. Wrist |
RT. Wrist |
RT. Thumb |
|
|
Improvement after six weeks |
38% |
38% |
51% |
42% |
42% |
32% |
50% |
70% |
41% |
20% |
0% |
20% |
0.43% |
|
|
Improvement after six weeks |
59% |
60% |
65% |
64% |
50% |
38% |
10% |
70% |
64% |
52% |
0% |
40% |
0.75% |
|
Table 5: Self-reported average improvement of each joint in terms of pain and function six weeks and six months after a single injection of ExoFlo.
Discussion
This preliminary investigator-led IRB study shows the safety primarily, and secondarily provides evidence of clinical efficacy in treating OA of the knee, shoulder, elbow, hip, ankle, or wrist with a single 2mL injection of a BM-MSC-derived EV product (ExoFlo). 6 months post-ExoFlo injection, the average Navy SEAL veteran improved 77% in BPI, 80% in ODI, 76% in LEFS, 51% in UEFS, and 77% in QD. All improvements were to a value of p<0.001. Most of the improvement (95%) occurred within the first 6 weeks post treatment. There were no complications or adverse events, minor or major, and no patient was made worse from the therapeutic injection. Four patients reported no significant improvement from the injection. One patient developed a cervical radiculopathy and one developed a lumbar radiculopathy that over-shadowed their OA symptoms in filling out the follow-up forms. Two patients did not improve clinically to the injection for unknown reasons. All of the joints injected are a di-arthrodial joint with a synovial lining and a joint capsule. The synovial capsule contains numerous synovial MSCs (more than found in bone marrow or adipose).
These MSCs are reported to have more chondrogenic potential than bone or adipose MSCs [28,29]. During the development of OA, pro-inflammatory and catabolic growth factors are produced by these synovial MSCs. This creates a chronically inflamed, painful, and degenerative joint environment. It has been reported that there are only, on average, 2,500 MSCs per milliliter of bone marrow concentrate (BMC) [27]. Despite the fact that there are very low numbers of MSC's present in BMC, there is increasing literature reporting the clinical efficacy of BMC used for the treatment of OA [12-16]. BMC/MSC cell survival or differentiation cannot explain this effect. One biological mechanism to explain the reported clinical efficacy is the release of acellular paracrine factors that regulate the osteoarthritic inflammatory response. Exosomes have been found to package many of the BMMSC secreted paracrine immunomodulatory molecules. Both exosomal protein and RNA content have been shown in vitro to alter immune cell proliferation, cytokine expression, and chemotaxis [30,31]. The small size of exosomes and the fact that they are not viable (unlike mesenchymal stem cells themselves) enables delivery of significantly higher and potentially more efficacious doses into the OA joint without the potential agonism of inflammation due to cell death and clearance observed in cell therapeutics.
The multi-faceted capacity of EV-based therapeutics such as ExoFlo, provides a clear therapeutic advantage. Unlike single small molecule drugs, the EVs complex biochemistry provides a multi-targeted approach to treat OA. Firstly, the secretome's immunomodulatory proteins can immediately target and interact with leukocytes and synoviocytes to decrease their pro-inflammation activity within the arthritic joint. The proteins stimulate mRNA transcription that encodes cellular instructions to produce anti-inflammatory chemokines, cytokines, and anabolic signals to chondrocyte progenitors. These are, in turn, released into the synovial fluid from the recipient cells. Secondly, the exosomes upon endocytosis deliver their mRNA and miRNA content into the recipient cells, which are then translated or used to inhibit pro-inflammatory factor production. In turn, the recipient cells generate an altered pro-healing secretome that they then secrete and use to reinforce the original therapeutic reparative signaling.
This IRB study's limitations include the small number of patients and the relatively short 6-month follow up. The IRB study was not randomized with a control group. Additionally, this population of retired Navy SEALS are conditioned soldiers that have a higher tolerance to pain than the general population, which could skew the subjective pain reduction results. The results of this study indicate it may be reasonable to consider an injection of acellular allogeneic bone marrow-derived ExoFlo into any joint with OA prior to a patient undergoing joint arthroplasty.
Conclusion
Thirty-three former Navy SEAL veterans underwent a single injection of an acellular allogeneic bone marrow-derived MSC EVIP (ExoFlo) into an OA knee (n=58), shoulder (n=32), elbow (n=16), hip (n=12)), ankle (n=8) or wrist (n=6). Six-month follow-up was obtained on all but one patient (97% follow-up). Every Navy SEAL veteran had four combat-related injured joints injected. At the 6-month follow-up, the average patient improved 77% in BPI, 80% in ODI, 51% in UEFS, 76% in LEFS, and 77% in QD. All improvements were to a value of p<0.001. 95% percent of the improvement occurred with the first six weeks. Adverse events included increased back ache for 24 hrs in one patient, increased joint pain in the injected joint for 24 hours in four patients, a change in bowel habits in one patient for 24 hours, and disturbed sleep for two nights in one patient. Limitations of this IRB study include the small number of patients and the relatively short six- month follow up. The IRB study was not randomized with a control group. These results indicate a 2mL ExoFlo injection into an OA joint is safe and clinically efficacious and should be considered prior to joint replacement.
Acknowledgments
The authors would like to acknowledge the Navy SEAL veterans for their keen interest in exosome-based therapy for the treatment of their combat-related joint injuries.
Conflict of Interest
The authors have no conflict of interest with this study.
References
- http://orthoinfo.aaos.org/topic.cfm?topic=A00389
- http://orthoinfo.aaos.org/topic.cfm?topic=A00377
- Jüni P, Reichenbach S, Trelle S, Tschannen B, Wandel S, et al. (2007) Efficacy and safety of intraarticular hylan or hyaluronic acids for osteoarthritis of the knee: A randomized controlled trial. Arthritis Rheum. 56(11):3610-3619.
- Karlsson J, Sjögren LS, Lohmander LS. (2002) Comparison of two hyaluronan drugs and placebo in patients with knee osteoarthritis. A controlled, randomized, double-blind, parallel-design multicentre study. Rheumatology (Oxford). 41(11):1240-1248.
- Kotevoglu N, Iyıbozkurt PC, Hız O, Toktas H, Kuran B. (2006) A prospective randomised controlled clinical trial comparing the efficacy of different molecular weight hyaluronan solutions in the treatment of knee osteoarthritis. Rheumatol Int. 26(4):325-330.
- Raman R, Dutta A, Day N, Sharma HK, Shaw CJ, Johnson GV. (2008) Efficacy of Hylan G-F 20 and Sodium Hyaluronate in the treatment of osteoarthritis of the knee-A prospective randomized clinical trial. Knee. 15(4):318-324.
- Reichenbach S, Rutjes AW, Nüesch E, Trelle S, Jüni P. (2010) Joint lavage for osteoarthritis of the knee. In: Reichenbach S, ed. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2010:CD007320.
- WS Toh, CB Foldager, M Pei, JH Hui. (2014) Advances in mesenchymal stem cell- based strategies for cartilage repair and regeneration, Stem Cell Rev. 10(5):686e696.
- S Meirelles Lda, AM Fontes, DT Covas, AI Caplan. (2009) Mechanisms involved in the therapeutic properties of mesenchymal stem cells, Cytokine Growth Factor Rev. 20(5-6):419-427.
- R Hofer, RS Tuan. (2016) Secreted trophic factors of mesenchymal stem cells support neurovascular and musculoskeletal therapies. Stem Cell Res Ther. 7 (1): 131.
- Freitag J, Bates D, Boyd R, Shah K, Barnard A, et al. (2016) Mesenchymal Stem Cell Therapy in the Treatment of Osteoarthritis: Reparative Pathways, Safety and Efficacy- A review. BMC Musculoskeletal Disord. 17:230.
- Im GI. (2018) Tissue Engineering in Osteoarthritis: current Status and Prospect of Mesenchymal Stem Cell Therapy. Biodrugs. 32:183-192.
- Garay-Mendoza D, Villarreal-Martinez, Bedolla GA, Pérez-Garza DM, Olivo CA, et al. (2018) The Effect of Intra-articular injection of autologous bone marrow cells on Pain and Function in Patients with Osteoarthritis. Int J Rheum Dis. 21:140-147.
- Murphy JM, Fink DJ, Hunziker EB. (2003) Stem cell therapy in a caprine model of osteoarthritis. Arthritis Rheum. 48:3464-74.
- Al-Najar M, Khalil H, Ajlouni JA, Antary EA, Hamdan M, et.al. (2017) Intra-articular Injection Injection of Expanded autologous bone marrow mesenchymal cells in moderate to severe knee Osteoarthritis is Safe: A Phase 1/11. J Orthop Surg. Res. 12:190.
- Beitzel K, Solovyova O, Cote MP, Apostolakos J, Russell RP, et al. (2013) The Future Role of Mesenchymal Stem Cells in the Management of Shoulder Disorders. Arthroscopy. 11:1702-11.
- Li Z, Wang Y, Xiao K, Weng X. (2018) Emerging Role of Exosomes in the Joint Diseases. Cell Physiol Biochem. 47(5):2008-17.
- Cheng L, Zhang K, Wu S, Cui M, Xu T. (2017) Focus on Mesenchymal Stem Cell-Derived Exosomes: Opportunities and Challenges in Cell-Free Therapy. Stem Cells Int. 2017: 6305295.
- Zhang S, Chuah SJ, Lai RC, Po Hui JH, Lim SK, et al. (2018) MSC Exosomes Mediate Cartilage Repair by Enhancing Proliferation, Attenuating Apoptosis and Modulating Immune Reactivity. Biomaterials Feb. 156:16-27.
- Pettine K, Dordevic M. (2019) The Biologic Treatment of Osteoarthritis with Mesenchymal Stem Cell Exosomes: The Future is Now. J Stem Cell Res Develop Therap5:1-5.
- RC Lai, F Arslan, MM Lee, NS Sze, A Choo, et al. (2010) Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury. Stem Cell Res. 4(3):214e222.
- RC Lai, RW Yeo, SK Lim. (2015) Mesenchymal stem cell exosomes. Semin Cell Dev Biol. 40:82-8.
- GW Hu, Q Li, X Niu, B Hu, J Liu, et al. (2015) Exosomes secreted by human-induced pluripotent stem cell-derived mesenchymal stem cells attenuate limb ischemia by promoting angiogenesis in mice. Stem Cell Res Ther. 6(1):10.
- C Lee, SA Mitsialis, M Aslam, SH Vitali, E Vergadi, et al. (2012) Exosomes mediate the cytoprotective action of mesenchymal stromal cells on hypoxia-induced pulmonary hypertension. Circulation. 126(22):2601-11.
- S Zhang, WC Chu, RC Lai, SK Lim, JH Hui, et al. (2016) Exosomes derived from human embryonic mesenchymal stem cells promote osteochondral regeneration. Osteoarthr Cartil. 24(12):2135-2140.
- Kellgren JH, Lawrence JS. (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 16(4):494-502.
- Pettine KA, Murphy MB, Suzuki RK, Sand TT. (2015) Percutaneous injection of Autologous bone marrow concentrate significantly reduces lumbar discogenic pain through twelve months. Stem Cells. 33:146-56.
- Koga H, Muneta T, Ju JY, Nagase T, Nimura A, et al. (2007) Synovial Stem cells are Regionally Specified According to Local Microenvironments after Implantation for Cartilage Regeneration. Stem Cells. 25: 689-96.
- Fan J, Varshney RR, Ren L, Wang DA. (2009) Synovium-Derived Mesenchymal stem cells: A new source for musculoskeletal regeneration. Tissue Engineering Part B Review. 15(1):75-86.
- Phinney DG, Pittenger MF. (2017) Concise Review: MSC-Derived Exosomes for Cell-Free Therapy. Stem Cells. 35:851-858.
- Marbán E. (2018) The Secret Life of Exosomes: What Bees Can Teach Us About Next- Generation Therapeutics. J Am Coll Cardiol. 71(2):193-200.

