Effect of Ultraviolet Photo functionalization on the Hydrophilic Capacity of Implants with Different Titanium Grades and Surface Treatments
Álvarez Hurtado1*, Betín Portacio2, Choles Cruz3 and Rivera4
1Lecturer in the specialty of Oral and Reconstructive Implantology, CIEO UNICIEO University Foundation, Bogota, Colombia
2Resident of the specialization of Oral and Reconstructive Implantology, CIEO UNICIEO Foundation, Bogota, Colombia
3Resident of the specialization of oral and reconstructive implantology, CIEO UNICIEO Foundation, Bogota, Colombi
4Lecturer in the specialty of Oral and Reconstructive Implantology, CIEO UNICIEO University Foundation, Bogota, Colombia
*Corresponding author: Alvarez Hurtado, Department of Oral and Reconstructive Implantology, CIEO UNICIEO University Foundation, Bogotá, Cra 5 #118-10, Colombia
Citation: Hurtado A, Portacio B, Cruz C, Rivera. Effect of Ultraviolet Photofunctionalization on the Hydrophilic Capacity of Implants with Different Titanium Grades and Surface Treatments. Genesis J Dent Rep. 1(1):1-9.
Received: April 22, 2025 | Published: May 10, 2025
Copyright© 2025 genesis pub by Hurtado A, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License. This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
Abstract
Purpose
To compare the effect of photo functionalization with Ultraviolet (UV) light on the surface hydrophilia of two implants with different grades of Ti (titanium) and surface treatments.
Materials and method
Materials and method: Twenty dental implants were used from two commercial homes with different degrees of Ti and surface treatment (Tapered short, Bio horizons Inc, United States-Grado de Ti: 5 -RBT, CIS X1 UniCis, UniCIEO, Colombia – Grado de Ti: 4-SBM). (Tapered short, Biohorizons Inc, USA - IT Grade: 5 -RBT, CIS X1 UniCis, UniCIEO, Colombia - IT Grade: 4-SBM). The implants were photo-functionalized with ultraviolet (UV) light (GC labolight LV III equipment, wavelength 380 to 510 nm) for 1 minute, and then, a drop of filtered water was applied to the apical area to evaluate the angle of contact of both types of implants and thus determine whether titanium grade and surface treatment had any influence on hydrophilia. A (canon EOS Rebel T7, 24.1 MP, canon Macro 100 mm) digital camera was used to photograph the implants after they were photofunctionalized and once the water drop was applied to determine the contact angle. Using the AUTOCAD program, from the photographs, the outline of the implant and the drop was delimited with the polyline command, and then, the angle was measured (in sexagesimal degrees) with the command for measuring the angle from the surface of the implant to the drop. A measurement was performed for each of the samples; to determine the angle of contact, the data were recorded using the data collection instrument for further analysis.
Results
The implants of Ti grade TI 4 presented a greater contact angle with a mean of 36.60° compared to the grade of TI 5 implants with a mean of 5.60° after being photofunctionalized.
Conclusions
Titanium grade treatment and surface treatment increase hydrophilia on implant surfaces exposed to UV light; however, more scientific research is needed to support this theory.
Keywords
Hydrophilia; Photofunctionalization; TI grade; Hydrocarbon contamination; Surface treatment.
Introduction
Protein absorption on the implant surface affects the biological response of the surrounding tissues; dynamic changes in the Ti surface energy change hydrophobic surfaces to hydrophilic ones upon exposure to biosystem fluids. However, the initial undesired hydrophobicity probably slows down the primary interactions with plasma proteins essential for peri-implant bone healing [1].
Photofunctionalization with ultraviolet (UV) light can clean TiO2 surfaces by mediated photocatalysis and direct UV-light decomposition, modify the hydrophobic surfaces by changing them into superhydrophilic ones, and modify the electrostatic charges on the implant surface, thereby improving the bioactivity of the implant [2].
Photofunctionalization is neither an additive nor a subtractive method of surface modification. Titanium implant surfaces, regardless of their experimental or commercial use, are chemically contaminated because of the inevitable and progressive deposition of hydrocarbons [3].
Photofunctionalization has a stronger influence on the speed of osseointegration in regular and complex cases than other factors such as patient age and sex, implant diameter and length, and other host site conditions. Photofunctionalization improves and accelerates the rate of implant stability development [4].
Photofunctionalization with UV light has proven to be an effective, simple, and low-cost mechanism; however, it has not been widely used, and information regarding its applicability and effects on various implant systems with different degrees of Ti and surface treatments is limited [5,6]. Several authors indicate that exposure to UV light significantly enhances osteogenesis in terms of active remodeling; simultaneously, inflammatory and osteoclastic responses are suppressed as a result of a significant increase in the anti-inflammatory cytokine IL-10 [7, 8].
This generates an even greater need for research in this area to obtain scientific evidence to highlight the benefits of this novel procedure in various implant systems. Therefore, the current study aims to determine the effects of UV light photofunctionalization on the hydrophilicity of the surface of implants with different titanium grades and surface treatments.
Materials and Methods
Twenty dental implants from two commercial companies with different TI grades and surface treatments were used (Tapered short, Biohorizons Inc, United States – TO grade: 5-RBT, CIS Implants System, Colombia – TI grade: 4-SBM) (Table 1).
|
IMPLANT |
BIOHORIZONS |
CIEO SYSTEM IMPLANTS |
|
MACRO-ARCHITECTURE |
Hybrid Body: Cylindrical -Conical |
Conical body |
|
TITANIUM GRADE |
Ti grade 5 Ti6Al4V |
Ti grade 4 (UNS R50700) |
|
THREAD DESIGN |
Self-tapping inverted trapezoidal thread with non-cutting edges |
Square thread on body. Inverted trapezoidal thread in the apical portion of the implant. |
|
SURFACE TREATMENT |
Resorbable blast texturing (RBT) |
Advanced selective system (Sand blast media and acid etching). |
These implants were photofunctionalized with UV light (GC labolight LV III unit, wavelength 380 to 510 nm) for 1 min, and then, a drop of filtered water was applied to the apical area to evaluate the contact angle in both types of implants to determine if the degree of titanium and the surface treatment had any influence on their hydrophilicity. A (canon EOS Rebel T7, 24.1 MP, canon Macro 100 mm) digital camera was used to photograph the implants after they were photofunctionalized and once the water drop was applied to determine the contact angle. The AUTOCAD design software (AUTOCAD Version 2015 Autodesk, Inc) was used to analyze the images obtained.
The procedure for preparing the samples for measurement consisted of the following stages: Cleaning and control of the elements, photofunctionalization, placement of the implants, application of the water drop on each of the implants and photography, angle measurement, and statistical analysis of the data. Cleaning of the Macro 100 lens was performed with microfiltered water and a microfiber cloth. The dental implants were exposed to UV light for a period of 1 min using a UV light device (GC labolight LV III equipment, wavelength from 380 to 510 nm) immediately before applying the drop of filtered water. The implant to be measured was placed on the sample holder with its axis of symmetry perpendicular to the latter using an implant holder. Thus, the implant to be measured was vertical, with its lower part upwards, to take the measurement in the flat area of the apical portion of all the implants. A 0.5 milliliter drop of ultrafiltered water was placed with a calibrated pipette on the implants. AutoCAD was used to delimit the contour of the implant and the drop using the command "polyline", and then, the angle was measured with the command "measure angle" (in sexagesimal degrees), from the surface of the implant to the drop. A measurement for each of the samples was performed to determine the contact angle. The data were recorded using the data gathering instrument.
Results
In the box plot of the contact angle after photofunctionalization with UV light (Graph 1) a variability between implants with one grade of titanium and surface treatment and another was observed. The size of the box corresponds to this variability; in the graph, we can observe that implants with titanium grade TI 4 and surface treatment of acid etching and sandblasting (sand blast media) presented a significantly higher variability than those with TI 5 and resorbable blast texturing (RBT) surface treatment.
Graph 1: In the box plot of the contact angle after photofunctionalization with UV light.
In graph 2, a high difference in the mean deviation between the two evaluated groups can be observed. The blue point corresponds to the mean in both groups. This mean is significantly higher in the group of TI 4 grade, acid etching and sand blasting (SBM) surface treatment.
Graph 2: A high difference in the mean deviation between the two evaluated groups can be observed. The blue point corresponds to the mean in both groups. This mean is significantly higher in the group of TI 4 grade, acid etching and sand blasting (SBM) surface treatment.
In the descriptive statistics table (Table 2), the data show Ti grade and the surface treatments to be compared, contact angle, and number of implants. The mean of the implants with TI 5 grade and RBT surface treatment was 5.6000 and for the implants with TI 4 grade and SBM + GA surface treatment was 36.60. The standard deviation for the TI 5 group and RBT surface treatment was 2.633 and that for the TI 4 SBM and GA group was 7.23. The minimum for the TI 5 group and RBT surface treatment was 2.000 and that for the TI 4 group and SBM and GA surface treatment was 29.00.
Table 2: Descriptive Statistics.
The median for the TI 5 group and RBT was 6.000, and that for the TI 4 group and SBM and GA was 39.00. Table 3, 4 and 5.
Table 3: Equality of variances was not assumed for this analysis.
| Ti grade | Surface treatment | N | Media | Standard deviation | Standard error of the meant |
| Ti 5 | RBT | 10 | 5.6 | 2.63 | 0.83 |
| Ti 4 | SBM+GA | 10 | 36.6 | 7.23 | 2.3 |
Table 4: Descriptive statistics: contact angle after photo functionalization with UV light.
|
Difference |
IC of 95% for the Difference |
|
-31,00 |
(-36,36; -25,64) |
|
Test |
|
|
Null |
|
|
Hypothesis |
H₁: μ₁ - μ₂ = 0 alternate |
|
Hypothesis |
H₁: μ₁ - μ₂ ≠ 0 |
|
T-value |
GL P-value |
|
12,74 |
11 0,000 |
Table 5: Estimation of the difference.
Implants of TI grade 4 and SBM and GA surface treatment presented a higher contact angle with a mean of 36.60 compared to the mean of implants of TI grade 5 and RBT treatment with a mean of 5.6000. These findings indicate that implants of TI grade 4 and SBM and GA surface treatment present a lower hydrophilicity.
Image 1:
Image 2:
Discussion
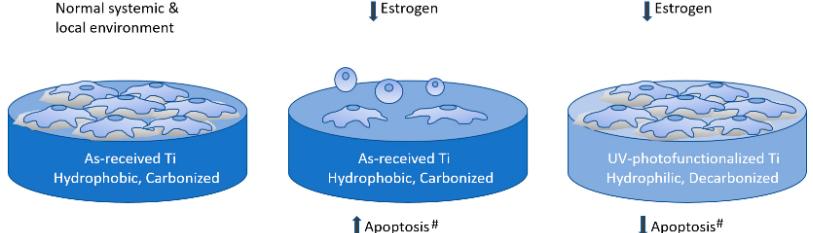
The results of the present study indicate that the effect of photofunctionalization with UV light on the surface hydrophilicity in implants varies according to the surface treatment. A higher hydrophilicity was observed in implants with TI grade 5 with sandblasting surface treatment by bombardment of a resorbable material, which provided a rough surface (Ra 75 μm). where it is quantified by means of the contact angle formed between the drop and the implant surface, showing a significantly lower average in favor of TI grade 5, considering that the lower the contact angle the higher the hydrophilicity, since the drop or fluid extends more on the implant surface.
A study aimed to determine the influence of UV light on the surface of titanium implants found that the application of UV light decreased the hydrophobicity of all the surfaces studied, although it did so to a greater extent on the surfaces to which a modification applied had been applied. This increase was more evident in samples manufactured with grade V titanium. In samples manufactured with titanium grade IV and those manufactured with grade IV and SLA treatment, this difference was less evident. This evidence coincides with the findings of the current study [9]. Modification of the physical parameters of a surface has an important effect on cell and tissue growth on the surface.
Because of the advancements in surface studies over the years, the influence of surface treatments on implants has been documented. These have evolved and have been described as additive and subtractive, and their biological advantages in implant therapy have been observed.
RBT surface treatment roughens the implant surface without leaving residual embedded particles or debris on the treated substrate. The material used for the RBT process is calcium phosphate. This is a highly resorbable and biocompatible material. The use of calcium phosphate as blasting material eliminates the need to use strong acids for the removal of blasting debris. Such surface technology provides excellent results, achieving optimal osseointegration and complete healing processes with almost zero chances of loosening.
Even the remaining particles are completely biocompatible and promote earlier bone growth. The most commonly used SLA dental implant surface is produced with alumina (sand) blasting and acid etching. The unique advantage of SLA is the creation of a highly porous two-tiered microsurface topography with valleys of 10 to 30 μm and craters with dips of 2 to 5 μm. The drawbacks of SLA are based on the use of bioincompatible alumina as the blast medium: alumina remnants on the surface are statistically unavoidable in this process, while the aggressive etching (usually even double etching) necessary to remove the alumina may considerably smoothen the implant surface, causing the surface to lose its roughness, which does not favor surface energy or loading. This agrees with the results of the present study which demonstrated higher hydrophilicity in implants with IT grade 5 with sandblasting surface treatment by bombardment of a resorbable material [10].
Another study aimed to compare whether UV treatment provided the same osteoconductive effects in commercially pure Ti as in T6aI4V, which is not pure titanium but an alloy, in rats. The study used implants made of Ti and T6AI4V, respectively, which were implanted in the tibiae of rats. The implants that were photofunctionalized showed higher Blc and BV indices [11].
Other authors suggest that photofunctionalization may extend the indications for simultaneous implant placement with bone augmentation, even in bones with severe anatomical compromise [12]. The essence of photofunctionalization is to clean titanium surfaces, which are spontaneously contaminated with natural hydrocarbons over time, to optimize the ability to establish osseointegration, regardless of the surface properties [13,14]. Carbon accumulation on the aged titanium surface is reduced to less than 20%, and the original form of titanium dioxide is exposed [15, 16].
Osteoblast attachment to the photofunctionalized titanium surface is markedly increased and, consequently, rigid bone integration with mostly 100% BIC has been achieved. Clinically, studies have reported that even with an initial bone support of less than 25% of the implant length or an ISQ of less than 30, photofunctionalization can achieve secure secondary stability. This is because the photofunctionalized implant achieves faster and superior osseointegration compared to as-received implants; the key essence of osseointegration on the photofunctionalized titanium surface is its superhydrophilicity, its absence of carbon, and its positively charged electrical state [17].
The titanium grade and surface treatment influences the hydrophilicity of implants when they are photofunctionalized with UV light. The study of these variables and how they can influence the hydrophilicity of the implant surface is fundamental for an increasingly safe and predictable clinical practice. Photofunctionalization with UV light has proven to be an effective, simple and low cost mechanism, but little diffused. There is little information regarding its applicability and its effects in diverse implant systems with different degrees of Ti [18].
Surface treatment is influential when applying UV light to clean the surface, which is interesting since the previously mentioned studies [19, 20]. demonstrated that the hydrophilicity obtained due to the elimination of the hydrocarbon layer by UV light improves the primary stability indexes, the application of implant with simultaneous bone augmentation even in complex cases, and improves the healing times.
Considering this, it would be favorable to apply this UV light on implants with different surface treatments to obtain better results or favorable responses and that increase to the maximum the hydrophilicity to be applied more efficiently. However, unfortunately, there is a scarcity of studies that support if the degree of Ti is influential or not in the increase of the hydrophilicity of the surfaces of implants photofunctionalized with UV light. This generates an even greater need for research in this regard to generate scientific evidence to highlight the benefits of this novel procedure in various implant systems.
Conclusion
According to the data presented, it can be concluded that surface treatment increases the hydrophilicity on implant surfaces exposed to UV light.
Acknowledgements
The author thanks Dr. M. Navarro for the support in photography. No grants were provided on support this study. The authors reported no conflicts of interest.
References
- Razali M, Ngeow WC, Omar RA, Chai WL. An integrated overview of ultraviolet technology for reversing titanium dental implant degradation: Mechanism of reaction and effectivity. Appl Sci. 2020;10(5):1–23.
- Atsumi M park S. Methods used to assess implant stability - current status. J Indian Prosthodont Soc. 2018;18:743–54.
- Accioni F, Vázquez J, Merinero M, Begines B, Alcudia A. Latest Trends in Surface Modification for Dental Implantology: Innovative Developments and Analytical Applications. Pharmaceutics. 2022;14(2):1–38.
- Dini C, Nagay BE, Cordeiro JM, da Cruz NC, Rangel EC, Ricomini-Filho AP, et al. UV-photofunctionalization of a biomimetic coating for dental implants application. Mater Sci Eng C. 2020;110(5):1–12.4.
- Hayashi M, Jimbo R, Xue Y, Mustafa K, Andersson M, Wennerberg A. Photocatalytically induced hydrophilicity influences bone remodelling at longer healing periods: A rabbit study. Clin Oral Implants Res. 2014;25 (6):749–54.
- Hirota M, Ozawa T, Iwai T, Mitsudo K, Ogawa T. UV mediated photofunctionalization of dental implant: A seven-year results of a prospective study. J Clin Med. 2020;9(9):1–12.
- Choi SH, Jeong WS, Cha JY, Lee JH, Lee KJ, Yu HS, et al. Overcoming the biological aging of titanium using a wet storage method after ultraviolet treatment. Sci Rep. 2017;7(1):1–12.
- Leon-Ramos JR, Diosdado-Cano JM, López-Santos C, Barranco A, Torres- Lagares D, Serrera-Figallo MÁ. Influence of titanium oxide pillar array nanometric structures and ultraviolet irradiation on the properties of the surface of dental implants— a pilot study. Nanomaterials. 2019;9(10):1–25.
- Funato A, Yamada M, Ogawa T. Success Rate, Healing Time, and Implant Stability of Photofunctionalized Dental Implants. Int J Oral Maxillofac Implants. 2013;28(5):1261–71.
- Moses O, Bengazi F, Ferri M, Gianfreda F, Velez J, Botticelli D, et al. Bioactivated Implant Surfaces Placed in Healed Sites or Extraction Sockets: A Preliminary Experimental Study in Dogs. Int J Oral Maxillofac Implants. 2022;37(5):963–70.
- Lee JH, Ogawa T. The biological aging of titanium implants. Implant Dent. 2012;21(5):415–21.
- Bosshardt DD, Chappuis V, Buser D. Osseointegration of titanium, titanium alloy and zirconia dental implants: current knowledge and open questions. Periodontol 2000. 2017;73(1):22–40.
- ecker M, Quabius S, Kewitz T, Hansen L, Becker G, Kern M, et al. In vitro proinflammatory gene expression changes in human whole blood after contact with plasma-treated implant surfaces. J Cranio-Maxillofacial Surg. 2019;47(8):1255–61.
- Miyauchi T, Yamada M, Yamamoto A, Iwasa F, Suzawa T, Kamijo R, et al. The enhanced characteristics of osteoblast adhesion to photofunctionalized nanoscale TiO2 layers on biomaterials surfaces. Biomaterials. 2010;31(14):3827–39.
- Ikeda T, Ueno T, Saruta J, Hirota M, Park W, Ogawa T. Ultraviolet treatment of titanium to enhance adhesion and retention of oral mucosa connective tissue and fibroblasts. Int J Mol Sci. 2021;22(22):1–17.
- Tateshima S, Kaneko N, Yamada M, Duckwiler G, Vinuela F, Ogawa T. Increased affinity of endothelial cells to NiTi using ultraviolet irradiation: An in vitro study. J Biomed Mater Res - Part A. 2018;106(4):1034–8.
- Kim MY, Choi H, Lee JH, Kim JH, Jung HS, Kim JH, et al. UV Photofunctionalization Effect on Bone Graft in Critical One-Wall Defect around Implant: A Pilot Study in Beagle Dogs. Biomed Res Int. 2016;2016:1–9.
- Funato A, Yamada M, Ogawa T, Yamauchi R, Itabashi T, Wada K, et al. Success Rate, Healing Time, and Implant Stability of Photofunctionalized Dental Implants. Int J Oral Maxillofac Implants. 2016;28(5):1261–71.
- Funato A, Ogawa T. Photofunctionalized Dental Implants: A Case Series in Compromised Bone. Int J Oral Maxillofac Implants. 2013;28(6):1589–601.
- 20. Roy M, Pompella A, Kubacki J, Szade J, Roy RA, Hedzelek W. Photofunctionalization of titanium: An alternative explanation of its chemical-physical mechanism. PLoS One. 2016;11(6):1–11.

