Immune Thrombocytopenic Purpura: a Case Report
Anoop V Somarajan1*, Athira Mohan S1, Ahamed Shabeer BS1 and Anusreeraj RS2
1Pharm D Intern, Ezhuthachan College of Pharmaceutical Sciences, Trivandrum, Kerala
2Assistant Professor, Department of Pharmacy Practice, Ezhuthachan College of Pharmaceutical Sciences, Trivandrum, Kerala
*Corresponding author: Somarajan AV, Pharm D Intern, Ezhuthachan College of Pharmaceutical Sciences, Trivandrum, Kerala
Citation: Somarajan AV, S Mohan A, BS Ahamed Shabeer, RS Anuseeraj. (2022) Immune Thrombocytopenic Purpura: a Case Report. J Stem Cell Res. 3(3):1-5.
Received: June 11, 2022 | Published: June 30, 2022
Copyright© 2022 genesis pub by Somarajan AV, et al. CC BY NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License., This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/JSCR.2021.3(3)-36
Abstract
Immune Thrombocytopenic Purpura also known as Idiopathic Thrombocytopenic Purpura or ITP, is an autoimmune disorder characterised by accelerated destruction and suboptimal platelet production that leads to reduced peripheral blood platelet counts. Females have a higher incidence than in Males with the ratio of 3:1. Here we present a case of 68-year-old female, with complaints of purpuric spots, ecchymosis, discolouration of tongue and history of melena. The treatment is initiated with IV dose of Corticosteroids followed by platelet infusions. Steroid dose must be tapered after one month of treatment schedule. Splenectomy is preferred in severe cases. ITP occurs because of platelet destruction abruptly by complex mechanisms in the immune system.
Keywords
Thrombocytopenic purpura; Purpuric spots; Ecchymosis; Splenectomy
Introduction
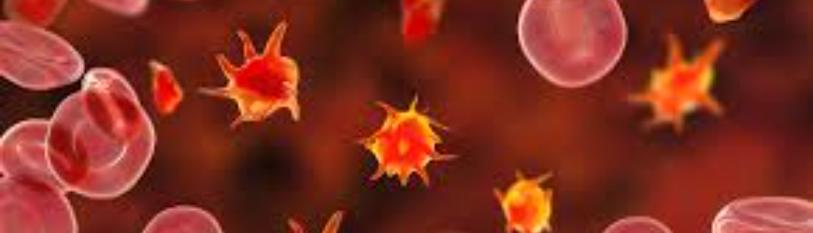
Immune Thrombocytopenic Purpura also known as Idiopathic Thrombocytopenic Purpura or ITP, is an autoimmune disorder characterized by accelerated destruction and suboptimal platelet production that leads to reduced peripheral blood platelet counts. Females have a higher incidence than in Males with the ratio of 3:1.ITP is mainly classified as acute and chronic. Acute ITP (short term) are those which lasts for <6 months where Chronic ITP (long term) lasts >6 months and seen commonly in adults. Based on cause ITP can be primary and secondary. Primary ITP occurs its own in the body and secondary ITP occurs as a result of and autoimmune conditions, chronic infections, pregnancy and neoplasm. Most common symptoms of Immune Thrombocytopenic Purpura include easy bruising & bleeding, petechiae (pinpoint in appearance), epistaxis, gingival bleeding, hematuria, melena, menorrhagia and prolonged bleeding during cuts and injuries. Incidence of mortality with ITP higher in elderly population. The ITP is consistently diagnosed with thrombocytopenia (< 20,000 cells/mm3), normal RBCs and normal WBCs.
Case Report
A 68-year-old female patient was encountered to the department of General medicine in a tertiary care hospital with complaints of purpuric spots, ecchymosis and history of melena. The patient had appearance of purpuric spots and discolouration of the tongue one day earlier. She had a medical history of Systemic Hypertension and was on Tab. TELMISARTAN 40mg. Her vitals were stable and patient was afebrile.
Examination revealed purpura and petechia positive on the abdomen. Patient also had a history of IPA in childhood. Also, she had osteoarthritis, hence was on mechanical knee pads for 1 year and was on PIROXICAM for 2-3 months. A Complete Blood Count (CBC) revealed patient had severe thrombocytopenia with a platelet count <20,0000 cells/mm3. Bleeding time, clotting time, Prothrombin and a PTT was normal. A provisional diagnosis of Thrombocytopenia, primary haematological can use was established (Figure 1).
Figure 1: Purpuric spots on lower limb.
The Blood picture showed normocytic normochromic anemia and marked thrombocytopenia. Stool observation showed positive blood content. A bone marrow infiltration was done and microbiological examination about Fungal/ AFB stain, AFB culture & fungal culture, Geno expert for MTB was done and showed no abnormal evidence. Bone marrow biopsy with IHC revealed increased number of mega karyocytes without morphological abnormality. No evidence of CLD on imaging but had a left renal cortical cyst was found. Based on the above investigation findings, the final diagnosis of ITP was made (Table 1).
|
Hematological tests |
Coagulation test |
|
WBC: 8080cells/mm3 |
Bleeding Time: 1min 45 sec |
|
Polymorphs: 70 % |
Clotting Time: 6min 40 sec |
|
Eosinophils: 2.6 % |
PT/INR: 1.12 |
|
Monocytes: 3.1 % |
aPTT: 24.7 |
|
Lymphocytes: 24.1 % |
BLOOD CHEMISTRY |
|
Platelets: 18,000cells/mm3 |
Ferritin: 140mg/ml |
|
RBCs: 335x 104/µL |
ALT: 29 U/L |
|
Haemoglobin: 9.9 g/dl |
AST: 47 U/L |
|
PCV: 33.5% |
Total Bilirubin: 1.05mg% |
|
RDW: 12.2% |
BUN: 58mg% |
|
ESR: 30mm/hr |
Creatinine: 1mg% |
Discussion
Immune Thrombocytopenic Purpura (ITP) also known as Idiopathic or Autoimmune Thrombocytopenic Purpura. In this condition, mostly bone marrow is in normal pattern. ITP is characterized by manifestations like petechiae, purpura, bleeding, ecchymosis, gingival bleeding, melena, brushing and other abnormalities. Both primary and secondary caused of haematological can lead to ITP. The incidence of ITP is higher in Females than in males. ITP occurs due to immune mediated mechanisms that destructs the platelets there by results in thrombocytopenia. When the platelet count drops below 20,000cells/mm3 the manifestation arises and the treatment is initiated to raise the platelet count. ITP occurs most commonly after immunization or viral infection.
Patients with ITP recover mostly from it before 6 months. Treatment protocol initiate with primary goal to increase the platelet count. For correct diagnosis, the exact cause of thrombocytopenia should be ruled out. Usually, drugs are given either intravenously or orally, intramuscular route is avoided due to its increased chance of bleeding into the skin. The treatment is initiated with IV dose of Corticosteroids, followed by IV Ig, platelet infusions. Steroid dose must be tapered after one month of treatment schedule. Splenectomy is preferred in severe cases.
Conclusion
ITP occurs because of platelet destruction abruptly by complex mechanisms in the immune system. Prompt diagnosis should be carried out in order to rule out other impending factors and to render appropriate treatment at the earliest.
References
1. Kuwana M, Okazaki Y, Satoh T, Asahi A, Kajihara M, et al. (2005) Initial laboratory findings useful for predicting the diagnosis of idiopathic thrombocytopenic purpura. Am J Med. 118(9):1026-33.
2. Terrell DR, Beebe LA, Vesely SK, Neas BR, Segal JB,et al. (2010) The incidence of immune thrombocytopenic purpura in children and adults: a critical review of published reports. Am J Hematol. 85:174-80.
3. Provan D, Newland A. (2002) Fifty years of idiopathic thrombocytopenic purpura management of refractor y ITP in adults. Br J Haematol. 118(4):933-44.
4. Gernsheimer T. (2009) Chronic idiopatic thrombocytopenic púrpura: mechanisms of pathogenesis. Oncologist. 14(1):12-21.
5. Sivakumar Y, Vandana.S, Kavya L, Dhanraj T. (2017) Idiopathic Thrombocytopenic purpura- A Case Report and an update of recent treatment modalities. J Scientific Dent. 7(1):24-27.

