Adipose-Derived Mesenchymal Stem Cells in the Treatment of Obesity
Megan Welsh and Vincent S. Gallicchio*
Departments of Health Science and Biological Sciences, College of Behavioral, Social and Health Science and College of Science, Clemson University, Clemson, SC, USA 29636
*Corresponding author: Vincent S. Gallicchio, Departments of Health Science and Biological Sciences, College of Behavioral, Social and Health Science and College of Science, Clemson University, Clemson, SC, USA 29636
Citation: Welsh M, Gallicchio VS. (2022) The Effect of Stem Cells on Bronchopulmonary Dysplasia. J Stem Cell Res. 3(1):1-18.
Received: March 08, 2022 | Published: March 30, 2022
Copyright© 2022 genesis pub by Welsh M, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License., This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/JSCR.2022.3(1)-29
Abstract
The growing obesity epidemic has presented many challenges in the treatment and prevention of the disease due to its multifactorial nature. The onset of obesity is complex and involves an intricate interaction between genetic, biologic, behavioral, socioeconomic, and environmental factors. Current treatment options focus on creating a negative energy balance where an individual burns off more energy than they consume. These treatments rely on drastic lifestyle changes that include increasing their amounts of physical activity and decreasing the amount of food consumed. In addition to these methods pharmacologic therapy can be used and when all else fails bariatric surgery such as a gastric bypass can be done. However, a common theme that occurs after these various treatments of obesity is weight regain after an initial weight loss. After treatment methods have been used some individuals regain more weight than they initially lost following the intervention. The need for an effective treatment option is essential to improving global health by decreasing obesity rates and its associated comorbidities. Therefore, new studies have emerged focusing on the use of adipose-derived mesenchymal stem cells as a therapeutic strategy for obesity. There have been several animal models that have shown that the use of adipose-derived mesenchymal stem cells could be an effective approach for treating obesity and its related comorbidities, however more studies need to be conducted in order to fully understand the mechanism.
Keywords
Obesity; Comorbidities; Adipose-derived mesenchymal stem cells; Treatment; Etiology
Introduction
Obesity is an epidemic that poses a long-term threat to the health and well-being of millions across the world and has a significant impact on global healthcare costs. According to WHO in 2016, there were more than 650 million adults who were obese. It has been predicted that if current trends continue then it possible that 38% of the world’s population will be overweight while 20% will be obese by the year 2030. One of the most alarming U.S.A. trends predicts that 85% of adults in the U.S. will be obese by 2030. In addition to a rising increase in obesity, there is an increase in associated disease because obesity alone is a serious risk factor in the development of things such as type 2 diabetes, dyslipidemia, hypertension, cardiovascular disease, stroke, myocardial infarction and even cancer [1]. One of the main outcomes that are associated with obesity is Metabolic Syndrome. This is a condition that is characterized by increased triglyceride levels, reduced levels of HDL, increased blood pressure, and an overall increase in blood glucose levels [2].
The multifactorial nature of the disease adds to the complexity of the treatment of the disease and has been a challenge for health personnel globally. The development of obesity is dependent on an individual's genetic, behavioral, socioeconomic, and environmental origins [1]. Even though this disease is multifactorial in nature, current obesity treatments mainly include changes like lifestyle modifications with diet and exercise, taking medication and when the previous methods do not work obese patients even undergo surgery [3]. These treatments do not encompass all of the factors that go into the development of the disease, therefore the current treatment options available are limited in their effectiveness [4,5]. Due to the limited results from current treatment options, there has been a shift on the types of treatment used to treat obesity and its comorbidities. A new focus has been on examining the effects that adipose-derived mesenchymal stem cells have on treating obesity and reducing the pathophysiological responses that it has on the body [7].
Etiology of Obesity
Initially obesity was considered to be a disease where individuals developed excess adipose tissue due to eating too much and exercising too little [1]. However, after years of studying this disease, it has been determined there are more factors that contribute to the development of obesity rather than just overeating and lack of exercise. Considering the classification of obesity as a multifactorial disease, it is evident there are a multitude of factors that are involved in the onset of obesity [1]. Some of the more obvious factors that are related to the onset of this disease are metabolic factors, diet, physical activity and a genetic predisposition [1]. The etiology of this disease is more complex and goes beyond diet and exercise to encompass environmental factors that contribute to an obesogenic environment and is even influenced by the central nervous system. While too much adipose tissue has very serious effects on health it also plays important roles in the regulation of total body energy homeostasis, reproduction, temperature, glucose balance, and immunity [5].
Energy balance and macronutrient effect on obesity
The idea that the body needs to maintain an equilibrium between energy intake and energy expenditure is vital in the etiology of obesity. The simple idea is that the number of calories you put in your body should be equal to the amount of energy that you expend or lose in a day. Burning more calories than you consume, or having a higher energy expenditure than energy intake, would lead to weight loss. Obesity is a consequence of consuming more calories than a person expends or having energy intake that exceeds energy expenditure. This is known as a positive energy balance and those that stay in a state of prolonged positive energy balance will eventually develop obesity [4].
In addition to the idea of energy balance in regard to energy consumption and expenditure with the development of obesity, macronutrient intake must also balance macronutrient oxidation. In order to determine whether an imbalance in the macronutrients in the body are involved in the development of obesity it is vital to look at the effect of each nutrient on the body and how it is stored in the body. Protein consumption should equate to 15% of dietary intake and is only representative of one third of the total amount of energy that is stored in the body. However, an increase in protein consumption does not necessarily lead to an increase in the amount of protein stored in the body. This increase would only arise from growth hormones like androgens and increased physical activity or weight gain. An overconsumption of protein therefore cannot lead to obesity because of the tight controls on protein stores but it is thought to have an effect on fat balance. Fat stores in the body are large and are a buffer for the body. The idea behind fat balance is the same as for overall energy balance. When someone enters a calorie deficit the calories come from fat stores and when someone consumes excess calories it ends up in fat stores [9]. Carbohydrates are another major macromolecule that the body needs, and this is usually the main source that living organisms get their energy from. Excess glucose consumption is usually stored in the form of glycogen in the liver and in the skeletal muscle tissues. Even though this is the main energy driver for organisms, glycogen stores are not abundant and contain around 500-1000g of glycogen. This stored glycogen also comes from the carbohydrates consumed that day so over the course of the day these stores are depleted. Similar to proteins, this tight control of carbohydrate stores signifies that excess carbohydrate consumption alone is not enough for obesity to develop. In contrast to proteins and carbohydrates, the fat stores in the body are large and contain around 6 times the energy found in protein stores. The fat stores act as an energy buffer for the body and correlates to small positive or negative energy balance meaning a deficit of 300 calories can come from fat stores but an increase in this many calories will be stored as fat. Therefore, most overconsumption of food that leads to an excess number of calories is stored as fat, increasing an individual's body fat [8].
Hormonal, neural and cellular influences on obesity
Hormones play a large role in the development of obesity. Not only do hormones regulate many important bodily responses including food cravings but they also influence adipocyte maturation. Some important hormone and cellular molecules that control this proliferation include insulin, insulin-like growth factor-1, and glucocorticoids. However, activation of the sympathetic nervous system (SNS) has the opposite effect and will inhibit adipocyte proliferation. In addition to their effects on the development of adipocytes, they also change the functionality of adipocytes. In large adipocytes that have undergone hypertrophy they are less sensitive to insulin which leads to chronic systemic inflammation that causes insulin resistance (IR) and type 2 diabetes that is linked to obesity [5].
Leptin is the hormone that suppresses the orexigenic pathway typically by sending signals of satiety after meals to decrease food consumption. Leptin is secreted by adipocytes so higher levels of leptin are generally seen in individuals with obesity. This abundant amount of leptin circulating in obese individuals is thought to cause a leptin resistance similar to that of insulin resistance. Leptin can cross the blood brain barrier and decrease the signals from NPY and AgRP. Individuals that are obese and have leptin resistance do not receive these signals to inhibit the effects of NPY and AgRP. Therefore, they stay in an orexigenic pathway always receiving signals to increase their food consumption [5].
Genetics and Epigenetic
The development of obesity is highly dependent on an individual's environment and genetics. Some individuals are predisposed to obesity based on their genetics and epigenetic modifications. There have been around 250 genes identified that are linked to the development of obesity with the fat mass and obesity (FTO) gene on chromosome 16 being the highest risk for developing obesity. Epigenetics looks at changes in the gene expression that occur without changes to an individual's DNA. Genetic and epigenetic alterations impact the body's metabolic pathways, neural pathways involved in homeostasis and regulation as well the body's appetite centers [9]. Genetic changes are inherited; however epigenetic changes are more complicated because they can occur at different times. However, there are specific times where these epigenetic changes are thought to occur the most frequently. During fetal development maternal over nutrition and under nutrition can affect the fetal metabolism [9]. The thrifty phenotype theory states that maternal under nutrition affects fetal insulin metabolism in such a way that when they are exposed to a nutrient rich environment, they are more at risk for developing type 2 diabetes. Mothers that are exposed to toxins or smoke regularly also cause epigenetic modifications in the fetus [9]. In addition to this, mothers who develop gestational diabetes, are underweight during pregnancy and who are young during pregnancy have also been linked to epigenetic changes that lead to the development of obesity. Furthermore, altered gut microbial flora with antibiotic use, paternal overnutrition and prediabetes as well as increased consumption of sugary drinks, saturated fats, sleep disturbances, and a sedentary lifestyle have all been linked to epigenetic changes that influence obesity [9].
There are three different types of obesity that are linked to various genetic pathways. Monogenic obesity is typically thought of as autosomal dominant or autosomal recessive forms of inherited obesity [9]. These mutations are typically single gene mutations that affect the leptin signaling pathway. Mutations in leptin can lead to activation of orexigenic pathways and inhibit anorexigenic pathways. Mutations can also occur in the NPY gene, ghrelin receptor mutations, and FTO mutations. Polygenic obesity is caused by the influence of a large number of genes whose effect is the promotion of weight gain [9]. Mutations can occur in CYP27A1, TFAP2B, PARK2, IFNGR1, UCP2 and UCP3 genes which are responsible for uncoupling proteins in brown adipose tissue (BAT) and skeletal muscle tissue [9]. These mutations also occur in ADRB1-3 which is responsible for beta-adrenergic receptors during lipolysis and SLC6A14 which influences tryptophan accessibility. This is important for production of serotonin which helps regulate appetite and energy balance [9]. This type of obesity is known as the common obesity and accounts for 60% of inherited cases of obesity. Polygenic mutations occur in genes that are involved in uncoupling proteins in skeletal and brown adipose tissue, and genes that code for beta-adrenergic receptors which influences energy utilization and lipolysis. Lastly mutations can be seen in the gene that regulates tryptophan levels needed for serotonin synthesis which then affects appetite and energy balance. Syndromic obesity is obesity that is caused by chromosomal rearrangements. This type of genetic obesity includes things like Prader-Willi syndrome, Bardet-Biedl syndrome, Fragile X syndrome and Cohen syndrome [9].
Epidemiology of Obesity
The role of epidemiologists is to ascertain the relationship between an exposure and the development of a disease in order to learn how to treat and prevent the disease. Due to the nature of obesity, it is extremely challenging to propose disease prevention measures because there are a lot of potential exposures that contribute to the disease. Obesity is classified as an epidemic so there have been many epidemiological studies examining the prevalence, trends, and risk factors of obesity in addition to the economic burden and morbidity and mortality associated with the disease [1].
In order to study obesity, it is vital that epidemiologists follow a specific criterion used to classify obesity [1]. The predominant criteria used to classify obesity is body mass index (BMI). An individual’s BMI is calculated by taking their body weight in kilograms and dividing it by their height in meters squared. According to the standard BMI criteria an individual is underweight if their BMI is <18.5 kg/m^2, normal if their BMI is 18.5-24.9 (125-168 lbs), overweight is 25.0-29.9 (169-202 lbs), obesity class I is 30-34.9 (203 lbs or higher), obesity class II 35-39.9 and obesity class III is 40 or higher [1]. BMI is the most widely used classification system because of its simple ascertainment; however BMI is flawed in its inability to distinguish between adipose tissues or lean tissue [4]. In addition to BMI other methods involve analyzing waist circumference (WC) and waist-to-hip-ratio (WHR). These two methods are used to measure an individual’s abdominal adiposity [1]. Visceral fat is most often associated with abdominal fat and is far more dangerous than subcutaneous fat. Visceral fat is metabolically active and surrounds itself around organs and can cause metabolic dysregulation which can lead to things like cardiovascular disease [1]. There are other more accurate ways at measuring body composition including skinfold thickness, bioelectrical impedance, hydrodensitometry (underwater weighing), dual-energy X-ray absorptiometry, ultrasound, and magnetic resonance imaging. While these measurements are an effective assessment of body composition, they are more expensive and complex, so they are not used as frequently [4].
The overweight population accounts for around 37% of the burden of the disease worldwide [4]. In the 30-year gap from 1980 to 2014 the worldwide prevalence of obesity practically doubled. Women are more likely to develop obesity than men, in 2014 the prevalence of obesity in women was 40% while the prevalence of men was 38%. Another noteworthy trend that coincides with the prevalence of obesity is in relation to income levels of countries. Countries that have high and middle incomes have twice the rate of obesity compared to low-income countries [4].
Morbidity and Mortality
The obesity epidemic has been so complex not only due its multifactorial nature, but also from the abundance of co-morbidities that are associated with the onset of obesity. Therefore, a person with obesity not only requires treatment for obesity in itself, but also treatment for the various complications that arise from a prolonged state of being overweight [3]. Many of the comorbidities that are associated with obesity include Type II diabetes mellitus, cardiovascular disease, chronic kidney disease (CKD), non-alcoholic fatty liver disease (NAFLD), hypertension, dyslipidemia, arthritis, polycystic ovary syndrome, infertility, gastroesophageal reflux disease (GERD and even various types of cancers [2].
Type II diabetes (T2D) is very common in those that have obesity, with around 50% of people with the disease are also diagnosed with diabetes [2]. Based on the BMI scale as a measure of obesity for every 1 kg/ increase in individuals calculated BMI, their risk for developing T2D increases by 20%. Furthermore, the higher the initial BMI, the higher the risk of developing T2D. For example, there is a 100% increase in the risk of developing diabetes with a BMI between 27.2 and 29.4 and 300% increase in individuals with a BMI greater than 29.4. This positive correlation shows the significant impact that weight gain has on the risk of developing T2D. The pathogenesis of T2D in obesity is related to the large amounts of free fatty acids (FFAs) that are circulating throughout the bloodstream [2]. The high levels of circulating FFAs enable the development of reactive oxygen species (ROS) in the body which then leads to oxidative stress. The increased amount of ROS in the body inevitably leads to insulin resistance in cells [10]. Antioxidants are typically used by the body in order to decrease the ROS and get the body out of oxidative stress however a high fat diet is associated with a decrease in antioxidants such as glutathione but an increase in molecules such as NADPH oxidase which increases ROS. In addition to ROS causing insulin resistance and T2D it has other repercussions in the body. In skeletal muscle increased oxidative stress due to a high fat diet leads to greater peripheral insulin resistance in muscle cells and can eventually lead to ectopic fat storage in muscles. With an increase in the amount of circulating glucose and FFAs the pancreas becomes tired and can no longer produce enough insulin to keep up. This leads to hyperglycemia and dyslipidemia as well. Lastly, the increased insulin resistance in the cells of the body causes an increase in the production of pro-inflammatory cytokines and a reduced number of anti-inflammatory cytokines. This keeps the body in a state of chronic inflammation which can lead to even more devastating effects. Uncontrolled diabetes can lead to even more serious consequences than the initial onset of symptoms including peripheral vascular disease, retinopathy, nephropathy, neuropathy and even stroke [2].
Another common issue seen in association with obesity is metabolic syndrome [2]. This is characterized by having three out of 5 conditions: increased triglyceride levels, decreased levels of HDL, increased fasting glucose levels, hypertension and increased LDLs. Metabolic syndrome is often associated with the CVD in obese patients and commonly leads to cardiomyopathy which makes it harder for the heart to pump blood. In obese patients this is mostly characterized by left ventricular hypertrophy and diastolic dysfunction [2]. The type of fat that an individual has also influences the development of CVD in obese individuals. When an individual has more visceral fat than subcutaneous fat then it is a major cardiometabolic risk factor. The accumulation of visceral fat causes an increase in the production of pro-inflammatory cytokines and adipokines. These signaling molecules contribute to the development of CVD because of their ability to increase atherosclerosis and function as a cardio depressant. This low-grade systemic inflammation is one of the biggest contributors to CVD [2]. Obesity increases the amount of atherosclerotic plaque buildup, macrophage infiltration and plaque instability through this systemic inflammation [10].
In addition to CVD, obesity can lead to the development of chronic kidney disease (CKD). Similar to TDM, for every 5 kg/ increase in an individual's BMI, their chance of mortality being associated with chronic kidney disease increases by an alarming 60%. One of the biggest associations seen between obesity and CKD involves the secretion of albumin. Obese individuals develop increases in the amount of albumin excreted and this is an early indicator of renal impairment and even CVD [10].
Non-alcoholic fatty liver disease (NAFLD) includes hepatic steatosis, and non-alcoholic steatohepatitis (NASH). NAFLD is most often caused by obesity and insulin resistance and it is the most common cause of liver disease in the United States [2]. Around 91% of obese individuals have steatosis, 37% have NASH while only 10% show any indication of Cirrhosis [2]. The development of NAFLD is widely associated with obesity and they share many of the same risk factors. NAFLD is associated with an increased intake in energy, diet composition, sedentary lifestyle with decreased physical activity along with fat distribution. Visceral fat is more closely related to the development of NAFLD, and this correlation can be justified by determining an individual's waist circumference [11]. One of the proposed mechanisms explaining the development of a fatty liver in obesity involves inflammation of hypertrophic adipose tissue [11]. When adipose tissue grows and expands it becomes infiltrated with macrophages and pro-inflammatory cytokines therefore causing this tissue to become insulin resistant. This inhibits the insulin mediated suppression process of lipolysis which results in an increase in the amount of FFA that is released from adipose tissue. The portal hypothesis of fatty liver comes from the idea that FFAs are taken up directly into the portal vein and the liver where the hepatocytes take them up and bind them with coenzyme A (CoA) [11]. This produces fatty acyl CoAs that can then create hepatic triglycerides and further impair insulin signaling [11]. In addition to adipose tissue becoming insulin resistant upon expansion, inflamed adipose tissue will secrete more amounts of proinflammatory cytokines. These cytokines include TNF-α and IL-6 and they have the ability to inhibit the production of the adipokine known as adiponectin. The imbalance between the secretions of these proinflammatory cytokines and the insulin sensitizing adipokine are thought to be another link between obesity and fatty liver disease [10].
Current Treatment Options
Due to the widespread health complications that arise from the onset of obesity it is imperative to have treatment options that limit obesity and its associated comorbidities [3]. Since obesity is an increasing trend across the globe, prevention of these diseases is one of the most important ways of decreasing its prevalence. Obesity prevention techniques focus on encouraging people to eat and drink appropriate amounts based on their individual needs and exercising regularly [3]. Treatment options for individuals with obesity also focus on the same techniques used to prevent obesity. One treatment option is dietary therapy where obese individuals are given specialized diets based on their specific weight loss goals. These individuals can engage in nutritional counseling with a group or on their own, but it has been found that group sessions on nutrition counseling are more effective [3]. Since most obese individuals become obese due to a state of prolonged positive energy balance, a diet should focus on allowing the individual to enter a energy deficit. This is usually done with a diet aimed at creating a 500-calorie deficit per day by decreasing either fat or carbohydrate consumption or by decreasing both [3]. In addition to dietary therapy increased exercise is also recommended as a potential treatment option for obese individuals. In order for exercise to be effective at reducing the amount of fat mass in an obese individual, they must exercise for more than 150 minutes per week where major muscles groups are used at a moderate to high intensity for a long work duration [3].
Other treatment options for obesity include weight reducing drugs and in extreme cases surgical intervention [3]. It is recommended that drug therapy be done in conjunction with other treatments such as diet and exercise therapies. The main drug that is recommended is orlistat. This should be used in individuals with comorbidities who have a BMI above 28 or in individuals with a BMI who have not seen beneficial effects with diet and exercise therapies alone [3]. Other drug therapies are not recommended for treatment because there is not much evidence that they are effective, and the benefits are not worth the risk of taking them. These drugs include amphetamine, diuretics, human chorionic gonadotropin (HCG), testosterone, thyroxine, growth hormones, and dietary supplements [3]. Treatment for extremely obese individuals typically involves surgical intervention. Surgical intervention is more effective at reducing body fat, improving comorbidities related to obesity and has an overall decreased risk of mortality [3]. While surgical intervention is more successful than conservative treatment options such as diet, exercise and drug therapy it is only recommended if these conservative methods have been unsuccessful. Conservative therapy is considered unsuccessful if after 6 months of use it leads to less than 10% of weight loss in patients with grade II obesity (BMI ) and less than 20% weight loss in those with grade III obesity (BMI ) [3].
While these are current treatment options available to those that are obese, they are not great long-term. Weight regains often follows weight loss after implementation of various treatment options where the increased weight gain is often more than they originally lost through various treatment therapies [5]. Obese individuals who underwent diet therapy were found to be 1.9 times more at risk of obesity if they were on a diet once, 2.9 times more at risk if they dieted more than once and 3.2 times more at risk if they always dieted [5]. In addition to this, obese individuals often experience weight loss plateaus in diet therapies, so they are no longer seeing any weight loss past a certain point [5]. Although, surgical interventions had better outcomes than conservative methods after two years around 50% of patients who underwent a gastric bypass surgery experienced issues of weight regain. This biological set point is thought to be one of the reasons for this weight regain, and these changes that try to return the body back to its set weight can be seen in (Figure 1) [5].
Figure 1: The altered neuroendocrine signaling seen following weight loss that often causes the subsequent weight regain. These changes decrease energy expenditure, stimulate the body to eat until the body reaches the original set body weight [6].
When obese individuals lose weight with diet restriction, increased physical activity, or bariatric surgery it activates various processes in the body that lead to weight regain [5]. These neuroendocrine signaling adaptations following weight loss involve the orexigenic and anorexigenic pathways discussed previously. As individuals lose fat mass leptin levels in the body are reduced [5]. In addition to this, glucose, insulin and melanocyte stimulating hormone (MSH) are reduced. Reduced leptin levels lead to an increase in the NPY and AgRP signals of the orexigenic pathway that signal for increased food consumption. Low levels of glucose and insulin from increased physical exercise leads to an increased production of adenosine monophosphate kinase (AMPK) which also provokes the release of NPY and AgRP [5]. In addition to changes in neuroendocrine signaling systemic metabolic changes occur after weight loss that also led to weight regain [5]. The anorexigenic pathway increases energy expenditure by increasing SNS activation and the basal metabolic rate. However, after weight loss there is a decrease in SNS stimulation, and secretion [5]. Triiodothyronine ( ) is a thyroid hormone that is regulated by thyroid stimulating hormone (TSH). It is responsible for increasing metabolic activity, carbohydrate metabolism, and it causes lipolysis and oxidation of fatty acids [5]. Therefore, a reduction in this thyroid hormone and decreased SNS stimulation decrease overall energy expenditure [5]. These metabolic and physiologic changes that occur in the body following weight loss show how difficult it is for obese individual to lose weight even with current treatment options.
Stem Cell Treatments and Models
As previously discussed, current treatments of obesity are effective only in the short term, if they are even effective at all. This poses the issue of weight regain in obese patients after current treatment. Therefore, a new treatment option being explored is the through the extraction and allocation of Mesenchymal stem cells (MSCs), also known as multipotent stromal cells in obese individuals and animals. One meta-analysis reviewed multiple studies that looked at the effects of this treatment on mice models since there has not been any clinical human trials [7].
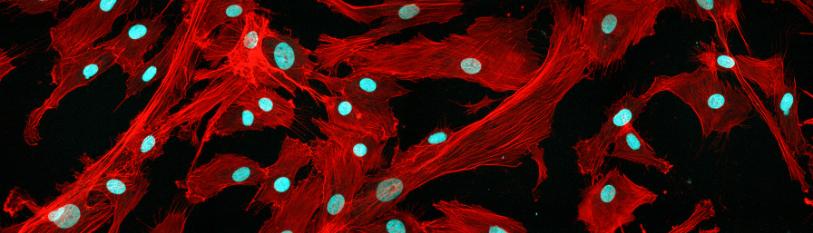
Mesenchymal stem cells are an ideal treatment for multiple types of disease, tissue regeneration and immune disorders because of their unique properties [7]. Mesenchymal stem cells have the ability to self-renew and differentiate into various types of cellular lineages [7]. A multipotent stem cell can become many different things that have vital functions to the body which is why they are so widely studied as treatment options for many pathophysiologies in the body [7]. While most MSCs are derived from the bone marrow, they can be extracted in various locations throughout the body. Stem cells can be obtained through an umbilical cord, amniotic fluid, placenta, skeletal muscle tissue, dental pulp, liver, synovial fluid, dermis of the skin, infra-patellar fat pad and lastly in adipose tissues [7]. The stem cells from adipose cells are termed Adipose-derived mesenchymal stem cells (AD-MSCs) and are the basis for the treatment of obesity due to their high proliferation rates, abundance in the body and their easy accessibility in the body. In addition to these attributes of AD-MSCs, they are known to have better physical maintenance long term than their close relatives bone marrow mesenchymal stem cells (BM-MSCs). Due to the large number of adipocytes that are generated by AD-MSCs the use of these in the treatment and management of obesity and its various comorbidities is a growing form of treatment [7].
Adipose derived mesenchymal stem cells have shown positive effects in the treatment of many different physiologies in the body and are known as a major source of cell therapy [12]. In order to obtain a large enough sample of AD-MSCs they must be extracted from fat tissue via liposuction and then allowed to proliferate in large numbers in a culture. Some of the effects seen with the use of AD-MSCs involve an improvement in tissue damage that arises from various diseases such as damage to ovaries due to chemotherapy, ischemia and neuronal apoptosis [12]. In addition to these improvements, other animal studies showed that when ASCs differentiated into osteoblasts in vitro and then were injected into mouse models they helped assist in bone formation. Other therapeutic effects that have been seen with these stem cells include production of alveolar bone, cementum, and periodontal ligaments when injected into damaged periodontal tissue. Lastly, ASCs have also shown to improve a fistula in an individual with Crohn’s disease [12].
The studies that have been conducted regarding the therapeutic effect of AD-MSCs have typically been done on diet induced obese (DIO) mouse models. These mice were given a high fat diet (HFD) and then AD-MSCs were used as a treatment to test their effectiveness at reducing weight levels, decreasing insulin resistance, and improving glucose homeostasis. One study examined 7-week-old mice where one group was fed a high-fat diet and the other group was fed a standard chow diet that did not cause weight gain [12]. After 20 weeks, DIO mice weighed significantly more than mice fed with chow. DIO mice were also shown to have decreased glucose tolerance and decreased insulin sensitivity. In order to determine whether intravenous infusion of ASCs could reduce obesity and insulin resistance the DIO mice received an injection of ASCs. The weight in DIO mice was slightly reduced but not enough to be significant. However, blood glucose levels of DIO mice treated with ASCs were significantly reduced. Furthermore, glucose disposal was increased in the DIO mice 2 weeks after cell infusion and 6 weeks after cell infusion (Figure 2).
To determine the mechanism of glucose disposal after ASC injection stains of the pancreas were taken from chow fed mice, DIO mice, and DIO mice injected with ASCs. The DIO mice showed reduced amounts of pancreatic β-cell area compared to chow fed mice [12]. However, mice injected with ASCs had preserved β -cell area of the pancreas proving that β -cell loss from a high fat diet is prevented after injections with ASCs. Levels of inflammatory cytokines were also measured in all three types of mice and showed increased levels of inflammatory cytokines such as TNF-α, F4/80, and IL-6 in the DIO mice compared to chow fed mice. However, ASC injected mice showed reduced amounts of TNF-α and F4/80 compared to the DIO mice. One of the major mechanisms associated with the protective effects of injection of ASCs involves the reduction of inflammatory cytokines in the pancreas. This reduction of proinflammatory cytokines limited the amount of inflammation in the pancreas which could have led to the preservation of β -cell mass in the pancreas [12]. Treatment of DIO mice with ASCs also showed protective effects on the liver with increased hepatic steatosis, and decreased numbers of fat cells. Furthermore, mice injected with ACSs showed a decrease in the size of adipocytes in adipose tissue suggesting that ASCs can lead to a reduction in the size of adipocytes brought on by a high fat diet. DIO mice also showed increased serum triglyceride levels and decreased levels of HDL [12].
Figure 2: Examined the difference in glucose disposal and insulin sensitivity in DIO mice and DIO + ASC mice at 2 weeks and 6 weeks post intravenous injection. 4a and 4b show improved glucose disposal 2 weeks after injection but 4c and 4d show no difference in insulin sensitivity at 2 weeks. 4e and 4f show significantly faster glucose disposal in DIO + ADS mice and 4g and 4h show slightly better insulin sensitivity in DIO + ADS mice [13].
However, DIO mice treated with ASCs had significantly reduced triglyceride levels and increased HDL levels. ASCs injections are also thought to have protective effects from inflammation of the liver. Normally, DIO mice have decreased expression of InsR (insulin receptor) and PPAR𝛾 (peroxisome proliferator-activated receptor 𝛾) genes, and increased expression of inflammatory cytokines like IL-6 and F4/80 in the liver [12]. The InsR and PPAR𝛾 genes are associated with insulin resistance whenever there is decreased expression of these genes. However, DIO mice injected with ASCs showed an increased expression of InsR and PPARy and a decreased expression of inflammatory cytokines in the liver. Therefore, another proposed mechanism for the effects seen in obese mice when treated with ASCs could be from insulin sensitizing effects [12] (Figure 3).
Figure 3: Examines the differences in the number of cytokines and metabolic dysregulation indicators between DIO, DIO + ASC, and CHOW fed mice. Helps shows that the DIO + ASC mice show decreased triglyceride levels (a), increased HDL (b), increased insulin sensitivity (c), increased PPAR𝛄 (d), decreased IL-6 (e), decreased F4/80 (f), decreased NOD2 (g) and the expression of certain target genes in the liver by examining glyceraldehyde 3-phosphate dehydrogenase (h) [14].
Another similar study was conducted using DIO mice and mice that were fed a normal diet. There were four different groups of mice used including two types of DIO groups which included mice with HFD + ADMSC and HFD + MEDIA. The other two groups of mice were fed a normal diet (ND) and consisted of ND + MEDIA and ND + ADMSC. The two controls in the study consisted of the ND and HFD + MEDIA groups [15]. The use of ADMSC in the treatment of DIO mice in this study also had beneficial results. The use of ADMSC in DIO mice showed a decrease in fat mass and a slight increase in lean mass and free fluids. Similar to the previous study, a decrease in hyperglycemia after injection with ADMSC is evident in DIO mice as well as improved glucose tolerance [15].
The risk of developing CVD that is associated with obesity was also examined during the study by looking at levels of atherogenic index of plasma (AIP). AIP is a marker in the body that is a strong indicator of CVD. Levels of these were highest in the HFD + MEDIA group of the DIO mice. Furthermore, the DIO group that was treated with ADMSCs showed a significant decrease in these AIP levels similar to those seen in ND mice. This finding represents a possible anti-atherosclerotic component in the treatment of obesity with ADMSC, thereby limiting the risks of CVD development in obese individuals [15 (Figure 4).
Figure 4: Shows how treatment with ADMSCs in a HFD mouse can significantly reduce the amount out atherogenic index of plasma (AIP) in obese mice [16].
The proposed mechanism by which these ADMSC contribute to the treatment of obesity and its various effects involves the attenuation of pro-inflammatory cytokines. Obesity itself causes the activation of macrophages in the adipose tissue that releases pro-inflammatory cytokines such as TNF-ɑ and IL-6 [15]. These inflammatory cytokines are also associated with the development of diabetes and CVD often seen in conjunction with obesity. In the study, a decrease in these two pro-inflammatory cytokines was seen that had similar levels to those of ND mice. This decrease in these pro-inflammatory cytokines is the possible explanation for the decrease in blood glucose levels as well as the cardioprotective effects seen with the treatment of ADMSC [15] (Figure 5).
While intravenous injection of ADMSC has been shown to be effective at treating obesity induced effects such as decreased blood glucose, decreased triglyceride levels, increased HDLs and increased insulin sensitivity, intramuscular injection (IM) of ADMSCs has also proven to be effective [14,15]. Similar to the other studies, a DIO mouse model was used after feeding mice a high fat diet until they experienced hyperglycemia, hyperinsulinemia, increased body weight and increased triglyceride levels. However, a control group of mice that took daily oral treatments of metformin was used, which is a medicine typically used to treat high blood sugar. Intramuscular injection was used as opposed to intravenous injection due to the metabolic effects of secreted myokines from muscles [18]. Myokines released from muscle tissue are associated with increased insulin sensitivity, glucose uptake and fatty acid oxidation [19].
Figure 5: Mice treated with ADMSCs had reduced amounts of pro-inflammatory cytokines. [17]
In contrast to the previous effects of IL-6 discussed, whenever IL-6 is released as a myokine from muscle it acts as an anti-inflammatory as opposed to a pro-inflammatory. IL-6 secreted from muscle cells is also thought to have important cross talk with the pancreas which increases insulin secretion by the pancreatic β-cells [19].
After treating the DIO mice with IM injection of ADMSC there was a decrease in hyperglycemia as well as a decrease in systemic IR. In extreme cases of IR there is a decreased amount of GLUT4 protein in the muscles therefore it is thought that ADMSC causes an increase in GLUT4 expression in muscles and subsequently increases insulin sensitivity and decreases IR [18]. Using a homeostatic model assessment of IR (HOMA-IR) a significant decrease in IR was observed, as well as decreased triglyceride levels by using a triglyceride glucose index. Mice that were treated with ADMSC suspension and cultured medium experienced a decrease in the number of oxidized LDLs and a decrease in the pro-inflammatory IL-6 [18]. However, those treated with metformin and cell lysate did not experience any change. Obesity is associated with hypertrophy of beta cells as well as fat accumulation in organs like the liver, however mice treated with ADMSCs showed a decrease in both of these metabolic dysregulations. After examination of histological images of subcutaneous fat, liver and pancreas in the mice treated with ADMSCs showed a reduced number of macrophages in these organs further indicating the anti-inflammatory effects that treatment with ADMSCs can have [18].
COVID-19 and Adipose Tissue
In December 2019 the world was introduced to its first outbreak of COVID-19 in Wuhan, China. By March 2020, the World Health Organization had declared COVID-19, formally known as severe acute respiratory syndrome coronavirus 2, a global pandemic [20]. Throughout the duration of this epidemic, experts have come up with certain predictors that lead to poor health outcomes in people that develop COVID-19. These risk factors include older age, male sex, CVD, hypertension, diabetes and obesity [21]. Obese individuals that develop COVID-19 are associated with increased risk of admission into intensive care units, increased risks of requiring mechanical ventilation and increased risks of adverse cardiovascular events [13, 21]. Several studies have been conducted in order to understand the possible link between disease survival in obese individuals and how obesity itself contributes to increased risk of COVID-19 and poor outcomes [20,21].
It is thought that adipocytes may act as a reservoir inside the body that increases the spread of the virus, increases viral shedding, increases the immune response and also contributes to cytokine amplification [21]. COVID-19 has the ability to affect various organs in the body including the lung, heart, intestines, kidney, liver, pancreas, testis and now adipocytes in visceral fats [22]. As discussed earlier, adipose tissue is a very important endocrine organ that is responsible for various metabolic processes in the body as well as maintaining homeostasis. Adipocytes are responsible for the release of several adipokines which include adiponectin, visfatin, resistin, and leptin. These adipokines are responsible for homeostasis, controlling inflammation, regulating energy, immunological responses and leptin. However, visfatin, leptin and resistin are proinflammatory cytokines whose levels are increased in obese individuals [22]. In obese individuals’ adipocytes release even more pro-inflammatory cytokines such as TNF-ɑ, IL-1 and IL-6. IL-6 is largely linked to a “cytokine storm” that can occur after an immune response and is a strong predictor of mortality in COVID-19 patients [21]. The proinflammatory nature of these adipocytes is thought to be one of the reasons why it is targeted by COVID-19. In addition to this, it is theorized that adipocytes might be more susceptible to viral entry due to the expression of angiotensin converting enzyme 2 (ACE2) [20 ,22]. The use of ACE2 is the primary mechanism in which the virus is able to enter and infect host cells. The viral spike protein that is present on the viral envelope binds to its receptor, on the ACE2 enzyme, and releases enzymes that allow the virus to fuse with the plasma membrane and enter the cell via endocytosis [13, 22]. As a result of this, the renin-angiotensin aldosterone system that regulates blood pressure and blood volume is interrupted. This causes a variety of adverse effects such as hypertension, inflammation, fibrosis, vasoconstriction thrombosis and pulmonary damage [22]. ACE2 is found in many tissues in the body such as alveolar cells, kidney cells, myocardial cells, epithelial cells, pancreatic cells and adipocytes [20]. All of these cells have high rates of expression of ACE2 and some studies have shown ACE2 receptors are more abundant in adipocytes than in the lungs which show the increased risk obese individuals have and also helps explain how adipocytes can act as a viral reservoir for COVID-19 [20].
Interestingly enough, adipose derived mesenchymal stem cells are a treatment that has been researched for the possible use of treating COVID-19 patients [23,24]. While lots of treatments have been explored for COVID-19 the use of ADMSCs has received lots of attention because of their anti-inflammatory effects [23]. Cytokine storms and increased inflammation from COVID-19 can cause devastating effects, especially in obese individuals, however the use of ADMSCs could inhibit the inflammation and cytokine storm associated with COVID-19 patients. Early studies that been conducted in order to examine the effects of ADMSCs have seen improvements in lung function, protective effects on alveoli epithelial cells, suppression of an overactive immune system and increased tissue repair [23,24].
Conclusion
Obesity is a multifactorial disease that arises from a complex interplay of biologic, environmental, genetic, behavioral and socioeconomic factors. Current trends show that the obesity epidemic is worsening, and current treatment options are not having a strong enough impact on slowing down this disease progression. Current treatment options include diet restriction with diet therapies, increased physical activity, and drug therapies typically used along with diet and exercise treatments. Whenever these conservative treatments are unsuccessful extreme cases of obesity can attempt surgical interventions such as bariatric surgery. Although surgical intervention had the most promising effects, obese individuals often experienced weight regains after weight loss with these treatment methods. The body’s ability to return to its ideal biological set point weight is thought to activate physiological processes in the body that stimulate obese individuals to regain the weight they lost. Therefore, a new treatment with the use of adipose-derived mesenchymal stem cells is widely being studied as a way to decrease obesity and its related comorbidities. Thus far, treatment of obesity with ADMSC observed in mice has shown propitious results in treating various factors associated with obesity including insulin resistance, increased pro-inflammatory cytokine production, hyperglycemia, hyperlipidemia, NAFLD, atherosclerosis, glucose intolerance, and permit an increase in HDLs, insulin secretion, and other important regulatory molecules that help stabilize dysregulated metabolic pathways.
In light of current events, with millions of people being impacted by COVID-19 globally these findings could have profound impacts in treating those affected with the virus. The mechanism behind the virus and its impact on obese individuals is now widely studied. This is due to the increased mortality rate and health related complications observed when obese individuals become infected with COVID-19. The virus is able to use adipocytes as a reservoir for increased viral shedding by using the ACEII receptor to enter the hosts fat cells. It is hypothesized that the ACEII enzyme is found in the most abundance in an individual’s fat cells and when they are attacked by the virus it can cause similar dysregulation seen in obesity. Therefore, ADMSC are not only a promising treatment in obesity, but their overall regulatory effects can also allow them to be a new modality in treating those battling COVID-19.
References
- Hruby A, Hu FB. (2015) The Epidemiology of Obesity: A Big Picture. PharmacoEconomics. 33(7):673-689.
- Abdelaal M, Roux CW, Docherty NG. (2017) Morbidity and mortality associated with obesity. Ann Transl Med. 5(7).
- Wirth A, Wabitsch M, Hauner H. (2014) The Prevention and Treatment of Obesity. Dtsch Arztebl Int.111: 705-13.
- Romieu I, Dossus L, Barquera S, Blottiere HM, Franks PW, et al. (2017) Energy balance and obesity: what are the main drivers? Cancer Causes and Control. 28(3):247-58.
- Rogge MM, Gautam B. (2017) Biology of obesity and weight regain: Implication for clinical practice. Journal of the American Association of Nurse Practitioners. 29(S1):S15-29.
- Rogge M. (2017) Biology of obesity and weight regain: Implications for clinical practice. J Am Acad Nurse Pract Title. 2017:S15-29.
- Saleh F, Itani L, Calugi S, Grave RD, Ghoch ME. (2018) Adipose-derived mesenchymal stem cells in the treatment of obesity: A systematic review of longitudinal studies on preclinical evidence. Curr Stem Cell Res Ther. 13: 466-75.
- Galgani J, Ravussin E. (2008) Energy metabolism, fuel selection and body weight regulation Int J Obes. 32(7): 109-19.
- https://www.ncbi.nlm.nih.gov/books/NBK573068/
- Carbone S, Canada JM, Billingsley HE, Siddiqui MS, Elagizi A, et al. (2019) Obesity paradox in cardiovascular disease: where do we stand? Vasc Health Risk Manag. 15: 89.
- Stefan N, Kantartzis K Haring HU. (2008) Causes and metabolic consequences of fatty liver. Endocrine Reviews. 29(7): 939-60.
- Cao M, Pan Q, Dong H, Yuan X, Li Y, and et al. (2015) Adipose-derived mesenchymal stem cells improve glucose homeostasis in high-fat diet-induced obese mice. Stem Cell Res Therapy. 6(1): 1-3.
- https://stemcellres.biomedcentral.com/articles/10.1186/s13287-015-0201-3
- Cao M. (2015) Serum lipid levels and gene expression in livers.Stem Cell Research and Therapy.
- Jaber H, Issa K, Eid A, Saleh F. (2021) The therapeutic effects of adipose-derived mesenchymal stem cells on obesity and its associated diseases in diet-induced obese mice. Scientific Reports. 11(1): 6291
- Jaber H. (2021) Reduced Atherogenic index of Plasma. [image] Scientific Reports.
- Jaber H. (2021) Reduced number of pro-inflammatory cytokines. Scientific Reports.
- Shree N, Venkategowda S, Venkatranganna MV, Datta I, & Bhonde RR. (2019). Human adipose tissue mesenchymal stem cells as a novel treatment modality for correcting obesity induced metabolic dysregulation. International Journal of Obesity. 43(10): 2107–2118.
- Pedersen L, Hojman P. (2012). Muscle-to-organ cross talk mediated by myokines. Adipocyte. 1(3): 164-167.
- Lasbleiz A, Gaborit B, Soghomonian A, Bartoli A, Ancel P, et al. (2021) COVID-19 and obesity: role of ectopic visceral and epicardial adipose tissues in myocardial injury. Frontiers in Endocrinology. 990.
- Ryan PM, Caplice NM. (2020). Is adipose tissue a reservoir for viral spread, immune activation, and cytokine amplification in coronavirus disease 2019? Obesity. 28(7), 1191–1194.
- Khwatenge C, Pate M, Miller L, Sang Y. (2021). Immunometabolic dysregulation at the intersection of obesity and covid-19. Frontiers in Endocrinol. 12
- Rogers CJ, Harman RJ, Bunnell BA, Schreiber MA, Xiang C, et al. (2020). Rationale for the clinical use of adipose-derived mesenchymal stem cells for COVID-19 patients. J Translational Med. 18(1): 1-9.
- Shi L, Wang L, Xu R, Zhang C, Xie Y, et al. (2021) Mesenchymal stem cell therapy for severe COVID-19. Signal Transduct. Target Ther. 6(1): 1-5.

