A Novel Technique for Sacroiliac Joint Radiofrequency Ablation: Combining Ultrasound and X-Ray Annotation for Enhanced Precision and Patient Comfort
Arul James1, Manish Mittal2* and Ganesan Baranidharan3
1Consultant in Anaesthesia and Chronic Pain, George Eliot hospital, UK, MBBS, MD, FRCA, FFPMRCA
2Consultant in Anaesthesia and Chronic Pain, George Eliot hospital, UK, MBBS, FRCA, FFPMRCA, EDRA, EDAIC
3Consultant in Anaesthesia and Chronic Pain, Leeds teaching hospitals, UK, MBBS, MD, FRCA, FFPMRCA
*Corresponding author: Manish Mittal, Consultant in Anaesthesia and Chronic Pain, George Eliot hospital, UK, MBBS, FRCA, FFPMRCA, EDRA, EDAIC
Citation: James A, Mittal M, and Baranidharan G. A Novel Technique for Sacroiliac Joint Radiofrequency Ablation: Combining Ultrasound and X-Ray Annotation for Enhanced Precision and Patient Comfort. J Clin Pract Med Case Rep. 1(2):1-8.
Received: December 08, 2024 | Published: December 19, 2024.
Copyright© 2024 genesis pub by James A et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License. This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/JCPMCR.2024.1(2)-15
Abstract
The sacroiliac Joint (SIJ) is the largest axial joint in the body, with extensive sensory innervation. SIJ is a di-arthrodial joint. The primary role of the SIJ is to provide stability and offset the load of the trunk to the lower limbs. An extensive architecture of ligamentous structures provides the stability of the joint. The key differences between other di-arthrodial joints and sacroiliac Joints are the presence of fibrocartilage and hyaline cartilage, discontinuity of the posterior capsule and many ridges and depressions that minimize movement and increase stability. The sacroiliac joint is innervated anteriorly by the anterior rami of L4, L5 and superior gluteal nerve. The posterior innervation is by the posterior sacral network (PSN), which originates from S1 to S3 lateral sacral nerves derived from their respective posterior rami (with occasional contribution from S4 and L5).
Sacroiliac joint (SIJ) radiofrequency ablation (RFA) is used as a treatment modality to obtain prolonged pain relief for patients with SIJ pain. It has been shown that patients treated with SIJ RFA were approximately four times more likely to achieve ≥50% pain reduction at three months compared with sham treatment [5]. Our technique aims to offer a simplified, patient-friendly approach. This technique aligns with research indicating the necessity for innovative RFA methods to reduce procedural discomfort and resource utilization.
Keywords
SIJ (Sacroiliac joint); RFA (Radiofrequency ablation); PSN (posterior sacral network); TST (transverse sacral tubercles); PSF (Posterior sacral foramen)
Introduction
The sacroiliac joint is innervated anteriorly by the anterior rami of L4, L5 and superior gluteal nerve. The posterior innervation is by the posterior sacral network (PSN), which originates from S1 to S3 lateral sacral nerves derived from their respective posterior rami (with occasional contribution from S4 and L5). In one of the recent cadaveric studies, the lateral branches of S1 and S2 contributed to the posterior sacral network (PSN) in 100% of specimens, S3 in 88%, L5 in 8%, and S4 in 4% [1].
The horizontal distance from the center of each transverse sacral tubercle (TST) to the lateral margin of its respective posterior sacral foramen increases as we move down from S1-S3 [1].
- TST1 to S1: 5.1 ± 0.5 mm
- TST2 to S2: 6.6 ± 0.6 mm
- TST3 to S3: 9.4 ± 0.6 mm
The sacroiliac Joint (SIJ) is a recognized source of low back pain, with 10-27% incidence [2]. The one-month prevalence of low back pain is 28.5% [3]. The prevalence of chronic low back pain secondary to SIJ varies between 15-25% [4]. Non-interventional treatments, including pain self-management-based therapies, pharmacological treatments and CBT-based treatments, are trialed first to manage the pain. If pain persists, interventions like injections with local Anaesthetic and corticosteroids are offered to help achieve self-management.
Sacroiliac joint (SIJ) radiofrequency ablation (RFA)is used as a treatment modality to obtain prolonged pain relief for patients with SIJ pain. It has been shown that patients treated with SIJ RFA were approximately four times more likely to achieve ≥50% pain reduction at three months compared with sham treatment [5]. Various nerve ablation technologies for SIJ RFA have been described. These include conventional RFA, pulsed RFA, internally cooled RFA and cryoablation.
In addition to the above neuro-ablative technologies, there are different needle tip placement techniques described in the literature, ranging from unipolar, bipolar, multipolar, and palisade techniques. The placement of the needle tip is mainly referenced to the sacral neural foramina, from which the lateral sacral nerves emerge and travel laterally to the SIJ.
The different techniques described in the literature require multiple needles (more costly) and multiple needle entry points (more painful) and increase the time taken to do the procedure.
Studies have highlighted the efficiency of targeted RFA procedures in managing SIJ pain, demonstrating significant pain reduction and functional improvement in patients [6, 7]. These studies underscore the importance of technique precision and patient comfort in the success of SI joint interventions.
The surface of the sacrum is uneven. The sacrum is known to have dysmorphic changes in 5 –70 % of the population, including dysmorphic sacral foramina [8]. The edges of sacral foramina may not be easily identifiable in some patients, and the presence of bowel shadows makes it challenging to visualize.
In bipolar needle tip placements, the radiofrequency cannula (RFC) active tips need to be parallel to each other and within 1 cm to achieve optimal creation of thermos-ablative lesions. Due to the irregularity of the surface of the sacrum, it may be difficult to achieve parallel radiofrequency cannula tip placements requiring multiple re-directions, which will be time-consuming and painful. The RFC tip may be at different depths due to surface irregularity, which may not create an optimal thermo-ablative lesion.
In some practices, sedation or strong intravenous painkillers like IV paracetamol and fentanyl are administered as part of SIJ RFA to help with procedural pain; this increases recovery and discharge time.
In contrast, our technique aims to offer a simplified, patient-friendly approach. This technique aligns with research indicating the necessity for innovative RFA methods to reduce procedural discomfort and resource utilization.
Technique Description
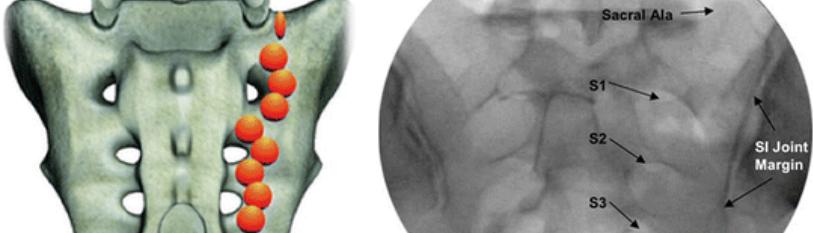
The technique is characterized by creating a unipolar strip lesion just medial to the SIJ, within 0.5 cm of the dorsal sacral surface, employing a single 18-gauge RFC with a 1 - 1.5 cm exposed tip. X-ray annotation guides RFC advancements of 1 - 1.5 cm, respectively. The strip lesion is created in a line between target areas A and B, described below and shown in (figure 1). Radiofrequency ablation (RFA), as explained in this article, targets the PSN as they pass over the transverse sacral tubercles (TST1-TST3) on the lateral sacral crest.
The patient is placed in a prone position. All sterile precautions are taken. An AP X-ray is taken to view the target SIJ and sacrum. Using a Curvilinear 2-5 MHz transducer, marking of the TST (1-4), posterior sacral foramen (PSF 1-4) and identification of any deep vessels is completed as shown in figures 1, 2, 3 and 4. Xray and USG both is used to complete the surface marking of needle alignment and trajectory.
Figure 1: Ultrasound image showing Transverse sacral tubercle (TST), Posterior sacral foramen (PSF) and Sacroiliac joint at S2 level in Transverse plane.
Figure 2: Ultrasound image showing Transverse sacral tubercle (TST), Posterior sacral foramen (PSF) at S3 level in Transverse plane.
Figure 3: Ultrasound image showing Transverse sacral tubercle (TST), Posterior sacral foramen (PSF) at S4 level in Transverse plane.
Figure 4: Ultrasound image showing, Posterior sacral foramen (PSF) in Saggital plane.
An RFC is inserted in a conventional way to create an RF neuro ablative lesion of the L5 dorsal ramus. A radio-opaque pointer is used to identify target area A, the area just medial to the inferior aspect of the posterior sacroiliac joint line seen in the X-ray. A 15 cm (curved) RFC and electrode usually help get the whole strip lesion with a single-entry point. The RFC entry point is 3 cm distal to target area A, where local anaesthetic is given. RFC is inserted and angulated to reach the initial target area A.
A Curvilinear 2-5 MHz transducer can be used to help get the orientation of the tip of the RFC parallel to the periosteum. Once this is achieved, a lateral X-ray is taken to confirm the needle tip position. The aim is to get the exposed tip of the RFC parallel to the posterior sacral surface, within a distance of 0.5 cm to the dorsal sacral surface. The tactile sensation of reaching the dorsal sacral surface is helpful as well. Sensory and motor testing are done to rule out radicular or sphincter stimulation. One ml of local anaesthetic precedes the RF thermos-ablation, performed at 80-90°C for 1.5– 2 minutes.
Target area B is the ipsilateral S1 sacral superior articular process and sacral ala junction. The annotation tool in the X-ray display monitor is used to draw a 1 cm / 1.5 cm line distal to the RFC tip along the required strip lesion pathway between target areas A and B as shown in figure 5. The distance measured can be calibrated to account for the magnification of the images obtained. This will accurately tell us how much the needle needs to be advanced.
The needle tip is moved superiorly by 1 cm / 1.5 cm along the AB strip lesion trajectory. The needle advancement and confirmation must be done in AP and lateral X-ray view as shown in figure 6. Infiltration of local an aesthetic as we advance helps with patient tolerability, followed by RF ablation.
This process is repeated, with advancements of the RFC equivalent to the length of the exposed tip, to cover the AB strip lesion, usually requiring 4-5 advancements to reach the junction of the ipsilateral S1 sacral superior articular process and sacral ala. With this technique, sometimes the posterior superior iliac spine prevents a straight AB strip lesion. Target area C is just medial to the PSIS.
Figure 5: X-ray of Sacro-iliac Joint (SIJ) AP view with annotations and needle trajectory.
Figure 6: Radiofrequency cannula being advanced using the annotation tool as a guide.
Where it is prominent. The strip lesion would then be created between target areas A and C first, followed by a strip lesion between areas C and B. A new needle entry point is rarely required for the second strip lesion between C and B.
Discussion
The literature mentions unipolar RFC placements for SIJ RF neuro-ablation. However, the SIJ RF neuro-ablation technique described in this article is a well-refined, easy-to-identify anatomical target-based technique that utilizes X-ray annotation tools and ultrasound as a guide.
According to CT scan measurements, the SIJ surface's average size was 7.36 cm [8]. The required AB strip lesion length was around 6 cm during our routine clinical practice.
The main proposed advantage of our SIJ RF technique is improved patient comfort and tolerance of the SIJ RF neuro-ablation procedure, which may otherwise require sedation or strong opioids for procedural pain relief.
Since only one RF electrode is required for this technique, the cost is significantly less compared to techniques utilizing multiple RF electrodes. Since the placement involves just one RFC at a time with subsequent advancements in a well-defined trajectory, fewer needle tip adjustments are required.
Figure 7: X-ray of Sacro-iliac Joint in lateral view with needle tip placement and annotation guide.
Which keeps the procedural time to a minimum, saving expensive theatre costs and time.
In our practice, the outcome following this technique has subjectively been found to be non-inferior to other techniques described.
References
- Roberts SL, Burnham RS, Ravichandiran K, Agur AM, Loh EY. (2014) Cadaveric study of sacroiliac joint innervation: implications for diagnostic blocks and radiofrequency ablation. Regional Anesthesia& Pain Medicine. 39(6):456-64.
- Hansen HC, McKenzie-Brown AM, Cohen SP, Swicegood JR and Colson JD et al. (2007) Manchikanti L. Sacroiliac joint interventions: a systematic review. Pain Physician.10:165–184.
- Macfarlane GJ, Beasley M, Jones EA, Prescott GJ and Docking R et al. (2012) The prevalence and management of low back pain across adulthood: results from a population-based cross-sectional study (the MUSICIAN study). Pain. 153(1):27-32.
- Cohen SP. (2005) Sacroiliac Joint Pain: A Comprehensive Review of Anatomy, Diagnosis, and Treatment. Anesthesia & Analgesia. 101(5):1440-1453.
- Yang AJ, Wagner G, Burnham T, McCormick ZL and Schneider BJ. (2021) Radiofrequency Ablation for Chronic Posterior Sacroiliac Joint Complex Pain: A Comprehensive Review. Pain Med. 22(Suppl 1): S9-S13.
- Cohen SP, Chen Y, Neufeld NJ. (2013) Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Rev Neurother. 13(1):99-116.
- Klessinger S, Casser H-R, Gillner S, Koepp H and Kolf A et al. (2024) Radiofrequency Denervation of the Spine and the Sacroiliac Joint: A Systematic Review based on the Grades of Recommendations, Assessment, Development, and Evaluation Approach Resulting in a German National Guideline. Global Spine Journal. 14(7):2124-2154.
- Weigelt L, Laux CJ, Slankamenac K, Ngyuen TDL and Osterhoff G. (2019) Sacral Dysmorphism and its Implication on the Size of the Sacroiliac Joint Surface. Clinical Spine Surgery. 32(3): E140-E144.

