Refractory Hyponatremia with Recurrent Simple Partial Seizure and Deterioration of Working Memory
Adel Ekladious*
1Associate professor of medicine, Faculty of health and medical sciences, University of Western Australia, 35/ Stirling Highway, Perth Western Australia 6009
2Royal Hobart Hospital 48 Liverpool street, Hobart, Tasmania 7000 Australia
*Corresponding author: Ekladious A, Associate professor of medicine, Faculty of health and medical sciences, University of Western Australia, 35/ Stirling Highway, Perth Western Australia 6009
Citation: Ekladious A. (2022) Refractory Hyponatremia with Recurrent Simple Partial Seizure and Deterioration of Working Memory. Adv Clin Med Res. 3(2):1-5.
Received: June 22, 2022 | Published: July 15, 2022
Copyright© 2022 genesis pub by Ekladious A. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/ACMR.2022.3(2)-32
Abstract
We present a 49-year-old female presented with recent onset of increasing forgetfulness, involuntary movement of the right arm and face with no loss of consciousness in addition to severe hyponatremia. Her past medical history included type 1 Diabetes mellitus’ graves’ disease, and primary progressive multiple sclerosis admitted few times to the hospital for treatment of hyponatremia, and involuntary movement of the right arm and face. She was diagnosed as a focal seizure due to low sodium, treated with hypertonic saline and levetiracetam, in other occasion was diagnosed as urinary tract infection due to neurogenic bladder due to MS, and inappropriate secretion of antidiuretic hormone, despite treatment of all possible differential diagnosis, her serum sodium did not normalize, MRI with and without contrast and DWI ruled out any stroke but showed high signal in temporal lobes, CSF study did not show any evidence of viral or bacterial infection, 14-3-3 protein was not detected.
Limbic encephalitis panel was performed from serum and CSF, which confirmed positivity for VGKC (Voltage gated potassium channel) and LG11, patient was treated with 1 gram methylprednisolone for five days followed by oral prednisolone with tapering doses over 6 months, in addition to weekly intravenous immunoglobulin for two months, patient recovered completely with no involuntary movement or seizures, sodium was normalized, patient scored 30 over 30 in minimental score assessment. LG11 antibodies should be a standard investigation in any patient presented with isovolumic hypo osmolar refractory hyponatremia.
Keywords
LG11; NMDA encephalitis; Fasciobrachial; Hyponatraemia
Case-Report
49-year-old lady presented to her GP because of difficulty with her memory, she started to struggle in her work as a tax Accounant. Her medical history included type 1 Diabetes Mellitus and hypothyroid graves disease. She took 16 units of Lantus at bed time, her recent HBA1c was 6.2, she never had hypoglycemia, she did not have any diabetic ketoacidosis before, she also took 100 ug L- thyroxine in the morning, her thyroid profile within normal, she does not smoke, did not drink alcohol and never used illicit drug, she was diagnosed with primary progressive multiple sclerosis [1-4].
The following investigations was ordered by her GP, full blood count, metabolic panel, ESR, CRP, liver function tests. Thyroid function teats, HBA1c, CT head, autoimmune panel, septic screen. Which came either normal or negative, two weeks later was seen in emergency because of involuntary movement of her left arm, wrist and left side of the face which lasted for 30 seconds, was given I mg glucagon intra muscular by ambulance, blood sugar at that time was 7mmol.
Metabolic panel at that time showed that sodium was 121mml, patient admitted to HDU and given 3% hypertonic saline, CT head with and without contrast was unremarkable, septic screen was unrevealing.
Repeated serum sodium next day was 129 mmol, urine sodium was 80mmol, Serum osmolality was 260, urine osmolality was 310, early morning cortisol, and Syncthen test was normal, patient was reassured and instructed to restrict her intake to 1.5 liter a day.
Three days later patient was admitted to near hospital because of 10 episodes of involuntary shaking of her left arm, wrest and face, each episode lasted 30 seconds, associated with progressive deterioration of memory, examination in emergency was unremarkable, blood sugar was 8 mmol, metabolic panel was unremarkable apart from sodium which was 118 mmol ((135-141mmol/L)), repeated CT Head was normal, patient admitted to high dependency unit, fluid restricted to 1 liter over 24 hours, 100 ml of 3% saline was administered, serum osmolality was 210mOsm/kg (285-295), urine osmolality 310, sodium in urine 90 mmol, repeated early morning cortisol, 30 and 60 minutes after Cynacthen was within normal, her thyroid function showed Euthyroid status.
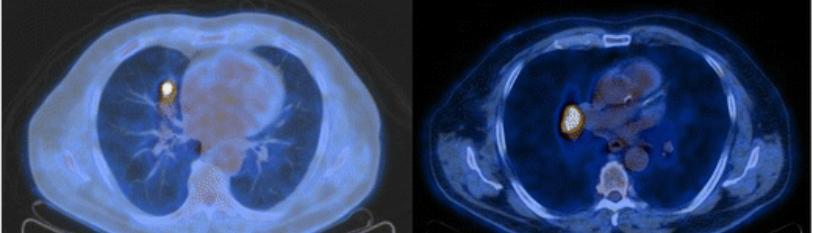
CT neck chest, abdomen and pelvis did not show any abnormalities, lumbar puncture showed A cellular fluid with mildly elevated CSF protein, gram stain culture, PCR for bacteria and virus was done. Serology for listeria, cryptococcus, bartonella and legionella in addition to SCF sugar and simultaneous serum sugar, all tests came either normal or negative, limbic encephalitis panel from CSF and serum was ordered, as well as tumor markers.
MRI with and without contrast revealed mild reduced volumes of both hippocampus, EEG showed mild slowing over the left temporal lobe. Tumor markers came negative, result of serum limbic encephalitis panel came positive for Calcium gated potassium channel and of Anti-Leucine -rich–Inactivated 1 Antibody (LG11) [5,6].
Patient received the diagnosis of LG11 autoimmune limbic encephalitis, patient was treated with 1 gram methylprednisolone for five days and continued on tapering dose of prednisolone over 6 months in addition to IV IGG o.4 gram /kg once weekly for 6 weeks, trimethoprim and sulphathiazole was added as a prophylaxis against pneumocystis jiroveci, calcium, vitamin D and Dunazemab added to medication for bone protection.
Patient seen weekly by her GP and every 6 weeks by neurologist and immunologist. All medication ceased after 6 months, nine months later patient reviewed by neurologist where patient still asymptomatic and metabolic panel was normal including serum sodium.
Discussion
Anti- Leucine -Rich Glioma- Inactivated 1 antibody Limbic encephalitis is a recently described disease. Characterized by gradual deterioration of memory, simple partial seizure, mainly unilateral affecting face and arm in the form of faciobrachial dystonic seizure which usually last up to 30 seconds or longer during one day, other types of seizure including myoclonic and tonic seizures can occur, the facio- brachial dystonic seizure is pathogenomic of autoimmune pathology that should prompt treatment with immunotherapy, that may prevent progression to severe limbic encephalitis, LG11 is a protein that forms a trans-synaptic VGKC through ADAM23 [7-9].
Seizure is recurring and stereotyping, it can occur up to 100 times a day, behaviour disorder had been described in the form of disinhibition, apathy, compulsive disorder, insomnia, hyponatremia had been described in most cases due to inappropriate secretion of antidiuretic hormone, hyponatremia is usually resistant and refractory even with restricted fluid, LG11 antibody occupy a region of VGKC channel complex.
LG11 is expressed in abundance in the hippocampus and temporal lobes. Testing for LG11 should be requested in both serum and CSF, positivity either in serum or CSF is enough for the diagnosis in the presence of the appropriate clinical manifestation [10-14].
Leucine -Rich, Gloma -inactivated 1 protein (LG11) IGG antibody is part of the Voltage - gated Potassium channel (VGKC) complex antibody, it is tested from serum and SCF with indirect fluorescent antibody assay utilizing Leucine – rich, glioma- inactivated 1 protein (LG11) transfected cell lines for the detection and semi-quantification of the LG11 IGG antibody, test had not been approved by the US food and drug administration yet. LG11 antibody limbic encephalitis is very uncommon autoimmune disease, it is classified as antineuronal surface antigen, antisynapetic protein – associated encephalitis, it is thought to be due to disruption of the dendritic spine density of dentate gyrus and thalamus neurons.
LG11 antibody is the most common cause of limbic encephalitis after anti N-methyl-D-Aspartate receptor (NMDAR) encephalitis, the most common manifestation of LG11 encephalitis is refractory simple partial seizure with poor response to antiepileptic treatment, other types of seizure can occur,
Patient can be admitted to intensive care unit because of epilepsy partial continua or status epeliptus, Seizures are usually missdiagnosed as a manifestation of hyponatremia, correcting hyponatremia does not cure seizures, and few patients might manifest with seizure without hyponatremia, many studies concluded that LG11 antibody encephalitis is a non-paraneoplastic disease, with Faciobrachial dystonic seizure consisting of few seconds’ contraction of the face and arm.
The cause of hyponatremia is not known but it is presumed to be due to excess secretion of antidiuretic hormone from the hypothalamus in the contest of isovolumic hypoosmolar hyponatremia. It is of paramount importance to exclude other types of autoimmune paraneoplastic limbic encephalitis like NMDA receptor paraneoplastic encephalitis, as these patients will be cured once the tumor are resected, when testing for autoimmune panel, phycision should have awareness to differentiate between the intracellular neuronal antigen which had a worse prognosis due to association with malignancy, (like anti-HU, anti Ri, anti ANNA1.2) from the neuronal cell surface /Synaptic antibody which have a better prognosis with immune therapy.
Phycisions should know that autoimmune antibody against Voltage Gated Potassium channel is not specific for the diagnosis of LG11 encephalitis as it can be seen in 5% of healthy people, and there is no evidence that VGKC titers are indicative of severity of the autoimmune disease. Other autoimmune diseases like hypothyroid graves and Addison disease should be ruled out as they can cause hyponatremia and seizures in rare occasions with severe hyponatremia and Hashimoto encephalitis.
There are no crystal-clear guidelines for treatment but all extracted from case series, case reports, expert opinion, there is no evidence from high quality multicenter randomized trails, Pulsed Corticosteroid therapy, followed by tapering dose of oral steroid over 6 months, Patients who could not tolerate or did not respond to steroid can be treated with plasmapheresis or IV immunoglobulin, it is important to have awareness that intravenous immunoglobulin can cause pseudo and true hyponatraemia due to Sucrose – induced translocation of water from intracellular to extracellular compartment. Few patients treated with steroid might need steroid soaring agent, patients diagnosed with LG11 autoimmunoencephalitis usually respond very well to immune therapy, relapse is rare if they treated promptly, with a good long-term prognosis, long term follow up is essential to make sure that relapse is diagnosed early and treated promptly [15].
Conclusion
Lucine-rich Glioma–Inactivated 1 (LG11) autoimmune encephalitis is common second to NMDA receptor antibody paraneoplastic encephalitis characterised by fasiobrachial dystonic seizure, hyponatraemia and cognitive dysfunction, early recognition, diagnosis and treatment has a very good prognosis and recovery. Every patient with Fasiobrachial seizure with cognitive impairment and hyponatraemia should be in the LG11 Pathway which includes, testing for LG11 antibody from CSF and serum, MRI, EEG, and ruling out another differential diagnosis which include viral encephalitis, Lymphoma, CNS vasculitis.
References
- Irani SR, Alexander S, Waters P, Kleopas AK, Pettingill P, et.al. (2010) Antibodies to Kv1 potassium channel-complex proteins Leucine-rich, Glioma inactivated 1 Protein and contactin- associated Protein 2 in limbic encephalitis, Morvan Syndrome and acquired neuromytonia. Brain. 9(1):2734-48.
- Brierley JB, Corsellis JA, Hierons R. (1960) Subacute encephalitisof later adult life mainly affecting the limbic areas. Brain. 83:357-368.
- Vincent A, bien CG, Irani SR, Waters P. (2011) Autoantibodies associated with diseases of the CNS: new developments and future challenges. Lancent Neurol. 10(8):73-78.
- Malter MP, Frish C, Schoene-Bake JC, Wandkinger KP, Stoecker W, et al. (2014) outcome of limbic encephalitis with VGKC- compleax antibodies: relationship to antigen specificity. J Neural. 261(9):1695-05.
- Van Sonderen A, Scheurs MW, Wirtz PW, Sillevis Smitt PA, Titulaer MJ. (2016) From VGKC to LG11 and CasPr2 encephalitis: the evolution of a disease entity over time. Autoimmune Rev. 15(10):970-74.
- Liu J, Li M, Li G, Zhou R. (2016) Anti-Leucine-rich Glioma- inactivated 1 antibody encephalitis, a case report and literature review. Exp Ther Med. 11(1):315-17.
- Messelmani M, Fekih- Mrissa N, Zaouali. (2015) Limbic encephalitis Associated with Leucine -rich glioma- inactivated 1 antibodies. Ann Saudi Med. 35(1):76-79.
- Krastinova E, Vigneron M, Le Bras P, Gasnault J, Goujard C. (2012) Treatment of limbic encephalitis with anti-glioma -inactivated 1(LG11) antibodies. J Clin Neurosci. 19(11):1580-82.
- Elancaster, J Dalmau. (2012) Neuroautoregulations-Pathogenesis, associated disorders and antibody testing. Nat Rev Neurol. 8:380-90.
- Asztely F, Kumlien E. (2012) The diagnosis and treatment of limbic encephalitis. Acta Neural scand. 126:365-75.
- Shin YW, Lee ST, Shin JW, Moon J, Lim JA, et al. (2013) VGKC-complex/LG11-antibody encephalitis: Clinical Manifistations and response to immunotherapy. J Neuroimmunol. 265:75-81.
- Andrade DM, Tai P, Dalmau J, wennberg R. (2011) Tonic seizres: a diagnostic clue of anti-Lg11 encephalitis? Neurology. 76(15):1355-7.
- Ramdhani RA, Frucht SJ. (2014) Isolated Chorea associated with LG11 antibody. Tremor other hypekinet. Mov (NY).
- Nilsson AC, Blaabjerg M. (2015) More evidence of neurocardiac prodrome in anti-LG11 encephalitis. J Neurol Sci. 357(1-2):310-1.
- Agazzi P, Bien CG, Staedler C, Biglio V, Gobbi C. (2015) Over 10-year follow up of Limbic Ebcephalitis associated with anti LG11 antibodies. J Neurol. 262(2):469-70.

