Pierre Robin Syndrome Case in Saudi Arabia: Case Report
Saja Alhaidar1*, Jawaher Alharbi2, Albandari Aldaws3, Najd Alsubaie4 and Rana Alasmari5
1,2Consultant Pediatric Dentist, King Saud Medical City
3,4,5General Dentist Riyadh, Saudi Arabia
*Corresponding author: Saja Alhaidar, Consultant Pediatric Dentist, King Saud Medical City
Citation: Alhaidar S , Aldaws A , Alsubaie N, Alasmari R. Pierre Robin Syndrome Case in Saudi Arabia: Case Report. J Oral Med and Dent Res. 6(1):1-7.
Received:December 23, 2024 | Published: January 24, 2025
Copyright© 2025 Genesis Pub by Alhaidar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are properly credited.
DOI: https://doi.org/10.52793/JOMDR.2025.6(1)-90
Abstract
Pierre Robin Syndrome (PRS) is a congenital condition characterized by micrognathia, glossoptosis, airway obstruction, and often a U-shaped cleft palate. This case report details the management of a 5-year-old Saudi boy diagnosed with PRS, presenting with multiple dental issues, malocclusion, impacted teeth, and feeding difficulties. There was no known family history of syndromes. Over the years, the patient underwent multiple surgical and orthodontic interventions, including mandibular distraction, cleft palate repair, and dental rehabilitation. The report highlights the complexity of treating PRS, with challenges such as airway management, delayed dental development, and significant malocclusion, requiring close collaboration between dental, orthodontic, and surgical teams. Long-term multidisciplinary follow-up, orthodontic treatment, and planned orthognathic surgery are essential for improving both functional and aesthetic outcomes. Early intervention, coupled with continuous dental supervision, plays a crucial role in managing the dental and craniofacial challenges associated with PRS.
Keywords
Congenital defects; Feeding problems; Micrognathia; Pediatrics; Pierre Robin syndrome; Pneumonia; Softpalate
Introduction
Pierre Robin Syndrome (PRS) is a congenital condition characterized by micrognathia or retrognathia, feeding difficulties, respiratory issues, cleft palate, and glossoptosis [1,2]. Although the exact prevalence of PRS is unknown, it is estimated to affect between 1 in 8,500 and 1 in 20,000 newborns [2]. There are theories suggesting that PRS may result from abnormal embryonic development in the caudal hindbrain [1]. PRS is a clinically well-defined subgroup of individuals with cleft lip and palate, though its precise cause remains unclear. It is often associated with other Mendelian syndromes, such as Marshall’s syndrome, velocardiofacial syndrome, and Stickler’s syndrome [3].
Recent genetic studies have indicated that PRS may be linked to the dysregulation of the genes SOX9 and KCNJ2, as evidenced by familial translocations with a breakpoint in the intergenic region between SOX9 and KCNJ2, as well as decreased expression of these genes in non-translocated PRS patients (4). Historically, airway obstruction in PRS has been reported to occur shortly after birth [5]. However, Ogborn and Pemberton refuted this, stating that airway obstruction in 5 of their 16 cases (30%) became apparent between the ages of 2 and 21 days [6]. Bull et al. noted that upper airway obstruction could manifest within the first month of life, though they provided no precise clinical details [7]. Later-occurring upper airway obstruction can have severe consequences, particularly after the initial hospital discharge. This case study explores such complications.
To date, no published studies from Saudi Arabia have examined the incidence or etiology of craniofacial anomalies. Among various facial syndromes, 72 cases (59.0%) were identified as having Pierre Robin sequence, 17 cases (13.9%) had Goldenhar syndrome, and another 17 cases (13.9%) had Van der Woude syndrome [8]. Given the rarity of published studies from Saudi Arabia, this case report presents the case of a 5-year-old Saudi boy diagnosed with PRS, who presented with multiple dental issues, malocclusion, impacted teeth, and feeding difficulties. There was no known family history of syndromes.
Case Report
A 5-year-old Saudi boy diagnosed with Pierre Robin Sequence presented with a chief complaint of restricted tongue movement, affecting speech, and significant dental decay. The patient’s history included palatoplasty, ear surgery, and the use of Continuous Positive Airway Pressure (CPAP) at a sleep clinic for respiratory support. There was no known family history of syndromes, allergies, or ongoing medication use. Since the age of 2, he had undergone multiple procedures, including cleft palate repair, tongue-tie release, and mandibular distraction, with the distraction device removed in January 2015. His mother noted a habit of finger-sucking during sleep.
Initial dental evaluation and management
During his first dental evaluation, restricted tongue movement and multiple carious teeth were observed, including stainless steel crowns (SSCs) from previous dental treatments. Further assessment by the Pediatric Department at King Saud Medical City revealed an open bite, dental crowding, caries in teeth #16 and #26, and poor oral hygiene. Radiographs, including periapical (PA) and orthopantomogram (OPG) views, were taken to assess the dental condition (Figure 1).
Figure 1: Periapical radiograph of tooth #36 showing its condition prior to treatment.
Preventive resin restorations (PRR) were applied to teeth #16 and #26, and the patient was referred to the orthodontics and oral and maxillofacial surgery (OMFS) departments for further management.
Figure 1.1: Periapical radiograph of teeth #46, and #85 prior treatment.
Figure 1.2: Orthopantomogram (OPG) of the patient at age 5, illustrating dental development and alignment at this stage.
Dental symptoms and evaluation at age 9
At the age of 9, the patient presented with intense pain in tooth #36. The extraoral examination revealed a retrognathic mandible, while the intraoral examination showed signs of plaque-induced gingivitis, occlusal imbalance, significant decay in tooth #36, dental crowding, and the absence of teeth #35, #37, and #38. An orthopantomogram (OPG) was ordered for a more detailed assessment (Figure 2). Tooth #36 was found to be non-restorable and was recommended for extraction due to pain upon percussion. The extraction attempt under local anesthesia (LA) was unsuccessful due to the patient's limited cooperation, prompting a referral for behavioral management and sedation with nitrous oxide.
Figure 2: Orthopantomogram (OPG) of the patient at age 9, illustrating dental development and alignment at this stage.
Orthodontic Observations
During follow-up appointments, orthodontic assessments revealed a convex facial profile, Class II malocclusion with a 7 mm overjet, a 5 mm open bite, a right-sided crossbite, and an impacted tooth #13. The patient also exhibited gingival overgrowth around the lower primary molars and the absence of teeth #35, #37, #38, #47, and #48. The proposed treatment plan included palatal expansion, with subsequent orthodontic treatment to be monitored after the eruption of the premolars.
Evaluation and treatment at age 10
At age 10, the follow-up evaluation showed healed surgical sites, a retruded mandible, fair oral hygiene, and improved sleep-related breathing patterns. A lateral cephalometric X-ray was taken (Figure 3). The patient underwent full-mouth dental rehabilitation under general anesthesia, which included fissure sealants on teeth #26, #34, and #45, preventive resin restorations (PRR) on tooth #16, and extractions of teeth #36 and #46 performed by the oral and maxillofacial surgery (OMFS) team.
Figure 3: Lateral cephalometric radiograph demonstrating the craniofacial profile, dental age and airway anatomy of the patient.
Orthodontic treatment at age 11
At the age of eleven, the patient commenced orthodontic treatment. The evaluation revealed a convex facial profile, severe skeletal Class II malocclusion attributed to a retrognathic mandible, a high mandibular plane angle, and incompetent lips. Intraoral examination showed congenitally missing teeth (#37, #38, #47, #48), impacted teeth (#33, #43), significant lower anterior crowding, an 8 mm overjet, a 4 mm anterior open bite, and a palatal fistula. Cone beam computed tomography (CBCT) and orthopantomogram (OPG) radiographs were obtained (Figures 4-6).
Figure 4.1: Extra-oral photographs at age 11, after the surgery.
Figure 4.2: Intra-oral photographs at age 11, detailing the dental arch, occlusion, and palate morphology after the surgery.
Figure 5: Cone beam computed tomography (CBCT) and orthopantomogram (OPG) scans showing detailed 3D imaging of craniofacial structures and dental anatomy of the patient.
Figure 6: Post-operative orthopantomogram (OPG) illustrating the dental and skeletal outcomes following treatment.
The patient was referred to an ENT specialist for evaluation of adenoid and breathing issues, and to pediatric psychology due to bullying related to his facial appearance at school. A referral to a nutritionist was also made as the patient's mother reported a decreased appetite.
The orthodontic treatment plan included creating space for the impacted tooth #13, bonding U4-4 brackets (excluding #13) (Figure 7).
Figure 7: Post-operative intra-oral and extra-oral photographs demonstrating the improvements in dental alignment, occlusion, and facial symmetry following treatment.
And using temporary anchorage devices (TADs) to visualize the lower premolars in order to make room for the impacted lower canines. Additionally, preparation for possible orthognathic surgery following orthodontic treatment was considered.
Results
Multidisciplinary management
The patient’s multidisciplinary care continued with a focus on addressing both functional and aesthetic needs, aiming to support oral health and psychosocial well-being.
Discussion
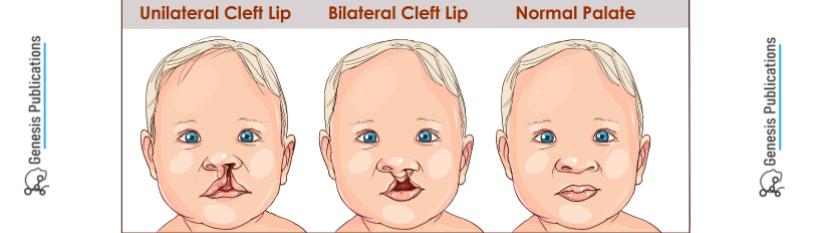
Pierre Robin Syndrome (PRS), also known as Pierre Robin Sequence, is primarily characterized by a triad of micrognathia (underdeveloped mandible), glossoptosis (posterior displacement of the tongue), and airway obstruction, often accompanied by a U-shaped cleft palate. From a dental perspective, PRS presents unique challenges that require careful management to ensure proper craniofacial growth, airway management, and oral function [9].
Mandibular underdevelopment is central to the pathophysiology of PRS. The small size of the mandible results in a posteriorly positioned tongue, obstructing the oropharyngeal airway and complicating breathing and feeding. Dental professionals play a vital role in diagnosing and managing craniofacial abnormalities that affect dental arch development, tooth eruption, and malocclusion [10].
When a cleft palate is present, it introduces additional dental challenges, such as impaired sucking reflex in infancy and an increased risk of dental caries due to difficulties in maintaining oral hygiene [11]. The lack of proper oral seals during early feeding can also hinder maxillary development. Dental professionals may collaborate in fabricating feeding plates to assist with feeding and minimize negative effects on oral health [11].
In our case, mandibular retrognathia led to severe Class II malocclusion and an anterior open bite as the child grew. Orthodontic interventions were performed to address these issues, and orthognathic surgery is planned as the final phase of treatment after the orthodontic phase is completed. A study by de Smalen (2017) concluded that partial tooth agenesis was observed in 47.8% of patients with non-syndromic Robin sequence (ns-RS) and 29.8% of those with non-syndromic cleft palate (ns-CP), with a greater prevalence in the mandible than the maxilla, especially in the ns-RS group. The teeth most frequently absent in both groups were the mandibular second premolars and maxillary lateral incisors [12]. In our case, teeth #13, #33, and #43 were impacted, while #35, #37, #38, #47, and #48 were congenitally missing. Since our case is associated with cleft palate, the patient underwent early surgical repair during the second year of life to aid in speech development and feeding. However, ongoing dental supervision was maintained to ensure proper maxillary arch development and address any dental complications. During this supervision, issues such as unilateral crossbite, open bite, and increased overjet were observed. A "bird face" appearance, reported by Hegde RJ [13], was also noted in this case, similar to the findings in our patient.
Conclusion
Pierre Robin Syndrome presents unique dental challenges related to mandibular underdevelopment, malocclusion, and cleft palate management. Early dental and orthodontic intervention is crucial for monitoring craniofacial growth, addressing malocclusion, and supporting feeding and speech development. Long-term follow-up is necessary to manage complications such as delayed tooth eruption and Class II malocclusion, as well as to plan for potential orthognathic surgery.
References
- Baujat G, Faure C, Zaouche A, Viarme F, Couly G, et al. (2001) Oroesophageal motor disorders in Pierre Robin syndrome. J Pediatr Gastroenterol Nutr. 32(3):297‐302.
- Guven DG, Senses DA, Subasi B, Yaman H. (2011) Absence of the epiglottis in an infant with Pierre Robin sequence. Int J Pediatr Otorhinolaryngol. 6(3):137‐39.
- Holder‐Espinasse M, Abadie V, Cormier‐Daire V, Beyler C, Manach Y, et al. (2001) Pierre Robin sequence : a series of 117 consecutive cases. J Pediatr. 139(4):588‐90.
- Jakobsen LP, Ullmann R, Christensen SB, Jensen KE, et al. (2007) Pierre Robin sequence may be caused by dysregulation of SOX9 and KCNJ2. J Med Genet. 44(6):381‐86.
- Dennison WM. (1965) The Pierre Robin syndrome. Pediatrics. 36(3):336‐41.
- Ogborn MR, Pemberton PJ. (1985) Late development of airway obstruction in the Robin anomalad (Pierre Robin syndrome) in the newborn. Aust Paediatr J. 21(3):199‐200.
- Bull MJ, Givan DC, Sadove AM, Bixler D, Hearn D. (1990) Improved outcome in Pierre Robin sequence: effect of multidisciplinary evaluation and management. Pediatrics. 86(2):294‐301.
- Aziza A, Kandasamy R, Shazia S. (2011) Pattern of craniofacial anomalies seen in a tertiary care hospital in Saudi Arabia. Ann Saudi Med. 31(5):488-93.
- Williams WN, Bevis RR. (1994) Dental and Orthodontic Management of Pierre Robin Sequence. Cleft Palate-Craniofacial J. 31(3):221-27.
- Antonarakis GS, Tompson BD, (2012) Fisher DM. Maxillofacial and Dental Development in Patients with Pierre Robin Sequence. Angle Orthod. 82(1):79-85.
- Berkowitz S. (2013) Cleft Lip and Palate: Diagnosis and Management. Springer.
- De Smalen A, Ross RJ, Wolvius EB, Van Wijk AJ, Ongkosuwito EM. (2017) Patterns of dental agenesis in non-syndromic Robin sequence and non-syndromic cleft palate. Eur J Orthod. 39(5):508-13.
- Hegde RJ, Mathrawala NR. (2010) Pierre Robin sequence: Report of two cases. J Indian Soc Pedod Prevent Dent. 28(4):326-30.

