Papillary Preservation Approach in The Treatment of Osseous Defects - A Report of 3 Cases
Akriti Mishra1*, Dipanjan Das2 and Avaneendra Talwar3
1,2,3Department of Periodontology, AB Shetty Memorial Institute of Dental Sciences, NITTE (Deemed to be University), Mangalore, Karnataka, India
*Corresponding author: Akriti Mishra. Department of Periodontology, AB Shetty Memorial Institute of Dental Sciences, NITTE (Deemed to be University), Mangalore, Karnataka, India.
Citation: Mishra A. Papillary Preservation Approach in The Treatment of Osseous Defects- A Report of 3 Cases. JOral Med and Dent Res. 5(4):1-7.
Received: August 2, 2024 | Published: August 18, 2024
Copyright© 2024 Genesis Pub by Mishra A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are properly credited.
DOI: https://doi.org/10.52793/JOMDR.2024.5(4)-71
Abstract
Managing osseous defects that are a result of periodontal diseases, especially when the preservation of the interdental papilla is critical, presents considerable clinical difficulties. Traditional flap designs, while providing necessary surgical access, often lead to post-operative soft tissue recession and loss of papilla, which negatively affects the aesthetics. Contemporary periodontal surgery focuses on not only removing periodontal pockets but also enhancing clinical attachment with minimal soft tissue shrinkage.The papillary preservation techniques have proven effective in minimizing tissue trauma while preserving soft tissues. This report discusses the application of these methods across three clinical cases, demonstrating their ability to reduce probing depths, encourage bone regeneration, and maintain aesthetic results.
Keywords
Periodontal surgery; Papilla preservation; Periodontal regeneration; Osseous defect.
Introduction
Periodontitis, a disease characterized by inflammation due to bacterial infections in the periodontal tissues, leads to the destruction of key structures like the gingiva, periodontal ligament, cementum, and alveolar bone. In 2018, the World Workshop Consensus introduced an updated classification system for periodontal diseases, focusing on staging and grading. Staging is used to determine the severity of the damage and the complexity of treatment required, while grading assesses the extent of harm, the risk of future damage, the likelihood of unfavorable treatment outcomes, and the disease’s connection to the patient’s overall systemic health [1,2].
Periodontal surgery becomes essential when persistent and active periodontal pockets exceeding 5mm are associated with intrabony defects. Such surgeries are conducted to access the deeper areas of the periodontal pocket and to repair the periodontal damage caused by the disease.[3] However, traditional flap designs in periodontal surgery often lead to the retraction of marginal tissues during healing, resulting in soft tissue defects in the interproximal areas.[4]
To address these issues, advanced techniques like microsurgery and the use of new bioactive regenerative agents, alongside papilla preservation techniques have been proposed. These methods aim to minimize wound, reduce flap reflection, and preserve the papilla.[5] The papilla preservation method (PPM), first described by Takei et al. in 1985, has been refined over the years, with notable modifications including the modified papilla preservation technique (MPPT).The modified-minimally invasive surgical technique (M-MIST).[6-9] These techniques are designed to minimize trauma to the papillary tissues, thereby preventing papillary collapse after surgery. However, the selection of a specific technique depends on the defect area in question and the patient’s aesthetic expectations.[10] This case report illustrates the application of various papilla preservation approaches in different clinical scenarios.
Case Presentation
Case 1
A 39-year-old systemically healthy female reported to the outpatient department with esthetic concerns and wanted her teeth to be properly aligned. However, a thorough oral examination revealed that her mandibular anterior teeth were mobile with deep probing depths. The patient was thus referred to the Periodontology department. Further radiographic examination revealed bone loss concerning the teeth 31 and 41. Upon periodontal examination, it was noted that tooth 31 was grade I mobile with a probing depth of 5mm (mesio-buccal) and attachment loss of 6mm (recession = 1mm) and tooth 41 was grade II mobile with a mesiobuccal probing depth and attachment loss of 7mm. The adjacent teeth 32 and 42 also had probing depths of 5mm each. The diagnosis, according to the 2017 classification, was made to be Localized Periodontitis Stage III Grade A. Non-surgical periodontal therapy was performed and further surgical procedure was explained to the patient concerning the mandibular anterior teeth. The patient reported back for the planned surgical procedure after 4 weeks. The interdental incision, between 31 and 41, was placed using MPPT as the distance was more than 2mm. A horizontal incision was, thus, made at the papilla base, followed by elevating a full-thickness flap lingually. Sulcular incisions were placed in the adjacent sites and full-thickness flaps were raised. The area was thoroughly described and the osseous defect was visualized.
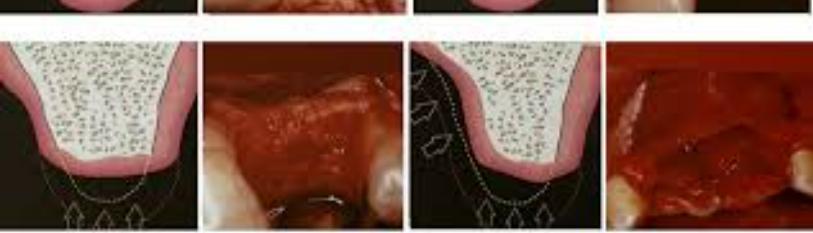
Figure 1: Occlusal view of the modified papilla preservation incision and defect visualization.
Xenograft (Geistlich Bio-Oss) was used to fill the defect site, followed by the placement of a resorbable collagen membrane (Geistlich Bio-Gide). Sutures were removed 2 weeks later. The tissues were stable 3 weeks post-surgery and even at 18 months follow-up, with 1mm of recession noted in both the treated teeth (31 and 41). Radiographic examination revealed bone fill and clinical examination showed reduced probing depth.
Case 2
A 35-year-old systemically healthy female reported to the department with the complaint of loose teeth in the lower front region. Upon examination, deep probing depth at the mesio-buccal and mesio-lingual sites (7-8mm) concerning tooth 41 with grade II mobility and recession of 1mm was noted. Furthermore, 5mm of probing depth (mesio-buccal) with grade I mobility concerning 42 was noted (Figures 6a,6b). Thediagnosis, as per the 2017 classification, was made to be Localized Periodontitis Stage III Grade A. Non-surgical periodontal therapy was performed and provisional splinting using a glass-fiber splint (Angelus Interlig) was done. The patient reported back for the planned surgical therapy after 4 weeks. The conventional PPM involves the placement of intrasulcular incisions facially and palatally, sparing the papillary region. A semilunar incision, extending 5mm apically from the line angles of the tooth, was made across the palatal papillary side and the flap is reflected buccally. After thorough debridement, the presence of an interdental crater was noted.
Figure 2: Interdental crater defect visualization post-flap reflection using conventional PPM
A combination of leukocyte-rich-platelet-rich fibrin (L-PRF) and xenograft (Geistlich Bio-Oss) was utilized to fill the defect site. The flap was finally sutured using cross-mattress sutures over the semilunar incision to achieve primary closure. Sutures were removed 2 weeks later. The tissues were stable at 1-month follow-up. Defect fill could be appreciated radiographically at the 3-months follow-up.
Case 3
A 45-year-old systemically healthy male reported to the department with the complaint of loose teeth in the upper right back region. Periodontal examination revealed a probing depth of 7mm on the mesio-palatal aspect of 16 and an attachment loss of 8mm (recession = 1mm) with grade I mobility. Tooth 15 had a probing depth of 5mm at the mid-palatal site.The buccal sites did not reveal significant probing depths. The diagnosis, according to the 2017 classification, was made to be Localized Periodontitis Stage III Grade A. After non-surgical periodontal therapy, the patient was recalled for the planned surgical procedure. M-MIST was used to raise the flap, while preserving the supra-crestal attachment and sparing the interdental papilla, by placing intrasulcular incisions connected by a horizontal incision, and creating a small window for palatal surgical access. Circumferential osseous defect involving the mesial and palatal aspects was noted, post-thorough debridement.
Figure 3: Circumferential bone defect visualization post-flap reflection using M-MIST.
Defect fill was achieved with xenograft (Geistlich Bio-Oss) and vertical mattress sutures were placed to achieve primary closure. Sutures were removed 2 weeks later. The tissues were stable 1-month follow-up. Defect fill could be appreciated radiographically at the 3-months follow-up.
Discussion
Treating osseous defects in periodontitis patients often poses significant challenges, particularly when the preservation of the interdental papilla is crucial. Conventional flap designs, although effective in providing surgical access, often lead to post-operative soft tissue recession and the loss of papillae, which can result in undesirable aesthetic outcomes and complicate the healing process. Modern periodontal surgery aims not only to eliminate the periodontal pocket but also to enhance clinical periodontal attachment while minimizing post-operative soft tissue contraction.[3,11] This case report highlights the importance of the papilla preservation approach in achieving minimal invasiveness and trauma to tissue, along with ease of access for carrying out the procedure.
The periodontal tissues are richly supplied by a complex network of supra-periosteal vessels and the plexus of the periodontal ligament, interconnected by intraseptal vessels through the Volkmann canals that traverse the alveolar bone. The success of soft tissue healing and the outcome of periodontal reconstruction are influenced by factors such as the extent of vascular damage caused by incisions, the flap design and suturing techniques to maintain slot space, the quality of wound closure, and the stability of marginal tissues during healing.[12,13] Papilla preservation techniques are specifically designed to protect the interproximal soft tissue. A retrospective analysis by Moreno-Rodriguez et al. in 2021 demonstrated that deep combined intrabony and supra-alveolar osseous defects can be effectively treated using papilla preservation techniques combined with a marginal approach, resulting in a significant reduction of periodontal pockets and an increase in clinical attachment.[3]
In this report, we utilized various papilla preservation techniques across three different cases, showcasing their versatility in addressing both aesthetic and functional concerns in the treatment of periodontal defects. The MPPT, employed in case 1, proved particularly beneficial in the anterior region where aesthetics are paramount. This technique preserves papillary integrity through careful incision placement and the use of barrier membranes, which support tissue regeneration and minimize recession.[8] The 18-month follow-up images revealed minimal post-operative recession and significant bone fill, underscoring the long-term effectiveness of this approach. This finding aligns with the work of Cortellini et al. (1996), who demonstrated superior results in bone regeneration and clinical attachment level gain using MPPT and barrier membranes.[14]
In case 2, a combination of the conventional PPM with L-PRF and xenograft was used to achieve defect fill. L-PRF has been shown to enhance healing by promoting soft tissue regeneration and reducing inflammation. The success of this approach, evidenced by the reduced probing depths (3mm) and bone fill at the 3-month follow-up, suggests that incorporating bioactive materials like L-PRF can improve clinical outcomes in periodontal surgeries. The result is consistent with the findings of Gupta et al. (2016), who reported that the papilla preservation flap technique not only produces an aesthetically pleasing tissue architecture but also offers a better approach for interproximal regenerative procedures, with PRF enhancing clinical outcomes.[15]
In Case 3, the M-MIST was used to treat an osseous defect in the posterior maxilla. This approach, which involves minimal flap elevation and the use of microsurgical techniques, has been shown to reduce surgical trauma and promote faster healing with fewer complications. The stability of the tissues and the reduction in probing depths at 3 months post-surgery in this case aligns with previous studies highlighting the advantages of minimally invasive approaches in periodontal regeneration. Have concluded in a 10-year follow-up of a randomized clinical trial that teeth with deep pockets associated with intrabony defects can be successfully maintained over the long term with either M-MIST alone or by adding a regenerative material. This result indicated that M-MIST is an effective periodontal surgical procedure for long-term beneficial outcomes [16]. Several studies have supported the effectiveness of papilla preservation techniques in minimizing post-operative tissue loss and promoting periodontal regeneration. Pasqualini et al.'s systematic review and meta-analysis (2024) concluded that such techniques significantly reduce papillary loss compared to traditional flap designs, though the choice of technique should be tailored to the specific defect and patient’s esthetic expectations. This is consistent with the outcomes observed in the present cases, where the choice of technique—whether MPPT, conventional PPM, or M-MIST—was based on the anatomic and aesthetic requirements of each case [10].
In summary, papilla preservation techniques represent a notable advancement in periodontal surgery, offering both functional and aesthetic benefits. The cases presented in this report illustrate the effective application of these techniques in achieving favorable clinical outcomes. Future research should continue to explore the long-term benefits of these approaches and refine the techniques to enhance their applicability in a wider range of clinical scenarios.
Conclusion
Papilla-preserving periodontal surgeries significantly decrease the surgical trauma in the soft tissues and the rates of wound failure after the surgery. As a consequence, many favorable clinical outcomes have been observed in the studies in which these techniques were applied, and the patient perception of the periodontal surgery also improved. However, the clinicians must estimate adequately the defect morphology to apply the most suitable surgical technique.
References
- Caton JG, Armitage G, Berglundh T, Chapple IL, Jepsen S, et al. (2018) A new classification scheme for periodontal and peri‐implant diseases and conditions–Introduction and key changes from the 1999 classification. J Clin Periodontol.45Suppl:S1-S8.
- Tonetti MS, Greenwell H, Kornman KS. (2018) Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Clin Periodontol. 89:S159-72.
- Moreno-Rodríguez JA, Ortiz-Ruiz AJ. (2021) Papilla preservation periodontal surgery in periodontal reconstruction for deep combined intra-suprabony defects. Retrospective analysis of a registry-based cohort. J Clin Exp Dent.13(8):e769.
- Jenkins WM, Wragg PF, Gilmour WH. (1990) Formation of interdental soft tissue defects after surgical treatment of periodontitis. J Clin Periodontol. 61(9):564-70.
- Harrel SK. (1999) A minimally invasive surgical approach for periodontal regeneration: surgical technique and observations. J Clin Periodontol.70(12):1547-57.
- Mishra A, Talwar A. (2024) Evolution of papilla preservation procedures- A Review. Clinical Dentistry (0974-3979).18(5):10-4.
- Takei HH, Han TJ, Carranza Jr FA, Kenney EB, Lekovic V. (1985) Flap technique for periodontal bone implants: Papilla preservation technique. J Clin Periodontol.56(4):204-10.
- Cortellini P, Prato GP, Tonetti MS. (1995) The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J Clin Periodontol.66(4):261-6.
- Cortellini P, Tonetti MS. (2009) Improved wound stability with a modified minimally invasive surgical technique in the regenerative treatment of isolated interdental intrabony defects. J Clin Periodontol.36(2):157-63.
- Pasqualini E, Castro F, Curado D, Martelete A, Heboyan A, et al. (2024) Minimally invasive periodontal regeneration with the buccal approach: a systematic review and meta-analysis of clinical studies. Evidence-Based Dent.25(1):54
- Cortellini P, Tonetti MS. (2007) A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intra‐bony defects: A novel approach to limit morbidity. J Clin Periodontol.34(1):87-93.
- Nobuto T, Suwa F, Kono T, Hatakeyama Y, Honjou N, et al. (2005) Microvascular response in the periosteum following mucoperiosteal flap surgery in dogs: 3‐dimensional observation of an angiogenic process. J Clin Periodontol.76(8):1339-45.
- McLean TN, Smith BA, Morrison EC, Nasjleti CE, Caffesse RG. (1995) Vascular changes following mucoperiosteal flap surgery: a fluorescein angiography study in dogs. J Clin Periodontol.66(3):205-10.
- Cortellini P, Prato GP, Tonetti MS. (1996) The modified papilla preservation technique with bioresorbable barrier membranes in the treatment of intrabony defects. Case reports. Int J Peri Res Dent. 16(6):11-3.
- Gupta D, Singh M, Agarwal MC, Gupta P. (2016) Conventional and modified papilla preservation flap (PPF) using bone graft and platelet rich fibrin (PRF): an attempt of management of soft tissues in an esthetic zone. Int J Con Med Res.3(1):105-7.
- Cortellini P, Cortellini S, Bonaccini D, Tonetti MS. (2022) Modified minimally invasive surgical technique in human intrabony defects with or without regenerative materials—10‐year follow‐up of a randomized clinical trial: Tooth retention, periodontitis recurrence, and costs. J Clin Periodontol.49(6):528-36.

