Orthopedic Complications of Sickle Cell Disease: A Retrospective Evaluation of 469 Patients in Port Harcourt, Nigeria
Friday Enwumelu Aaron1, Linda Dublin-Green2, Rex Friday Ogoronte Alderton Ijah3, Akpevweoghene Deborah Maduka4 and Hannah EOmunakwe5
1Associate Professor of Orthopedic Surgery, Department of Surgery, Rivers State University (RSU), and Consultant Orthopedic & Trauma Surgeon, Rivers State University Teaching Hospital (RSUTH), Port Harcourt, Nigeria.
2Lecturer and Consultant Hematologists, Department of Hematology & Blood Transfusion Medicine, University Teaching Hospital, Port Harcourt, Nigeria
3Senior Lecturer, Department of Surgery, Rivers State University (RSU), and Consultant General Surgeon, Rivers State University Teaching Hospital (RSUTH), Port Harcourt, Nigeria
4Lecturer and Consultant Hematologists, Department of Hematology & Blood Transfusion Medicine, University of Port Harcourt Teaching (UPTH), Port Harcourt, Nigeria
5Professor of Hematology and Blood Transfusion, Department of Hematology and Blood Transfusion, Rivers State University (RSU), & Consultant Hematologist, Rivers State University Teaching Hospital (RSUTH), Port Harcourt, Nigeria.
*Corresponding Author: Ijah RFOA, Senior Lecturer, Department of Surgery, Rivers State University (RSU), and Consultant General Surgeon, Rivers State University Teaching Hospital (RSUTH), Port Harcourt, Nigeria.
Citation: Aaron FE, Dublin-Green L, Alderton Ijah RFO, Maduka AD, Omunakwe HE. (2024) Orthopedic Complications of Sickle Cell Disease: A Retrospective Evaluation of 469 Patients in Port Harcourt, Nigeria. Adv Clin Med Res. 5(1):1-10.
Received: October 9, 2023 | Published: January 03, 2024
Copyright© 2024 genesis pub by Aaron FE, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives 4.0 International License., This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/ACMR.2024.5(1)-69
Abstract
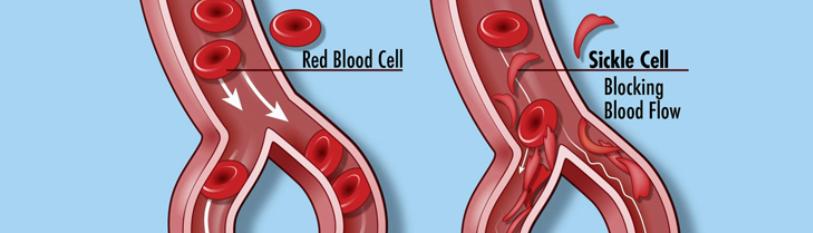
Background: Sickle cell anemia (SCA) is a hereditary blood disorder characterized by abnormal hemoglobin, leading to the deformation of red blood cells. There is growing impact of this condition on the musculoskeletal system. This study aimed to evaluate the Orthopedic complications in patients with SCA in Port Harcourt between July 2013 and June 2023.
Materials and Methods: A retrospective analytical study of Orthopedic complications in patients with SCA who presented to the Hematology clinics of two teaching Hospitals was conducted. Collected data was analyzed with the Statistical Package for Social Sciences.
Results: Among the 469 patients with SCA, 198 were males. The mean age of the study population was 25.21 years. The Orthopedic complications assessed included Avascular Necrosis of the Femoral head, Chronic leg ulcers (CLU), Osteomyelitis, and Osteoarthritis. A vascular Necrosis (AVN) of the Femoral head was observed in 50 (44.6%) patients. Chronic leg ulcers were present in 57 (50.9%) participants, while Osteomyelitis (OM) was identified in 14 (12.5%) patients. Osteoarthritis (OA) was the least common complication, occurring in only 3 individuals. The age group above 25years was statistically associated with development of Orthopedic complications especially for CLU and OM.
Conclusion: Orthopedic complications are common in SCA patients, with a vascular Necrosis of the Femoral head, Chronic leg ulcers, Osteomyelitis, and Osteoarthritis being the most frequently observed complications. These findings underscore the need for comprehensive management strategies and multidisciplinary care to minimize the impact of these complications on patients’ quality of life.
Keywords
Orthopedic Complications; Sickle Cell Disease; Port Harcourt; Nigeria
Introduction
Sickle cell anemia (SCA) is a hereditary blood disorder characterized by abnormal hemoglobin, leading to the deformation of red blood cells. This disease is most found in sub-Saharan Africa, East Mediterranean areas, Middle East, and India [1-2]. There has been a 13·7% global increase in the births of babies with sickle cell disease over a 21-year period from year 2000 and 2021 [3]. While the primary manifestations of SCA are related to the hematological system, there are divers clinical presentations with likelihood of the sickle cell disease patient being seen by the hematologist for outpatient care, the pediatrician or physician at the Emergency Department for sickle cell crisis, [4-5] by a General Surgeon for acute abdomen, [6-7] by a Nephrologists / Urologist for hematuria, [8] by the Orthopedic Surgeon for Orthopedic complications,[9-12]etc. Additionally, in managing any surgical condition in a patient with sickle cell anemia, special considerations or precautions are often taken for good outcome.[13-17]
While the standard care is known to be the use of analgesia, oxygenation, hydration, blood transfusions, and prevention of triggers of sickle cell crisis, [18] the use of a drug – Voxelotor, an inhibitor of polymerization of Hemoglobin S by increasing the oxygen affinity, has recently been shown to be very useful [19-22]. Orthopedic presentations and complications of sickle cell anemia has been reported in Eastern Nigeria, [23-24] Western Nigeria, [25-26] southern Nigeria, [27] and Northern Nigeria [28]. There is therefore growing recognition of the impact of this condition on the musculoskeletal system. Orthopedic complications among others are common among sickle cell disease patients in our practice, as reported in some studies in Nigeria [24-25, 27, 29]. Nigeria is known globally to have the largest cohort of sickle cell anemia (SCA), [27] and Port Harcourt is a cosmopolitan city with a high traffic of Nigerians due to petroleum oil and gas exploration and processing activities. This makes Port Harcourt to be home to many Nigerians, with the potential of physician encountering sickle cell disease patients and their complications. This study therefore explored orthopedic complications of sickle cell anemia patients as seen at the Hematology Clinics of Two Teaching Hospitals, Port Harcourt from July 2013 to June 2023.
Materials and Methods
Study Area: The study was carried out at The Rivers State University Teaching Hospital and the University of Port Harcourt Teaching Hospital, both being tertiary healthcare facilities in Port Harcourt, the capital of Rivers State, South-South of the Federal Republic of Nigeria.
Study Sites: The study site/setting was the Hematology Clinics of both Teaching Hospitals in Port Harcourt Nigeria.
Research Design: A retrospective analytical study.
Study Population: All patients (469) who were seen and treated at the study sites with orthopedic complications of Sickle Cell Anemia were included.
Sampling Method: Total population of sickle cell anemia patients with orthopedic complications as seen in the registers was used.
Study Instrument: The registers of the Hematology Clinics were used to obtain data that was imputed into a preformed designed for the study.
Study Variables: Patients’ age, sex, disease history (age of SCA diagnosis, known steady-state packed cell volume (PCV), history of blood transfusion, presence of siblings with SCA), and the orthopedic complications were the variables of interest.
Validity/Reliability of Instrument: The study data was scrutinized by all the authors for authenticity or otherwise before use.
Data Analysis: Data obtained was formed into tables and analyzed using the Statistical Package for the Social Sciences (SPSS) version 20.0. The Fishers’ Exact (p-value) test was used for the association between age / sex and orthopedic complications.
Results
|
Variable |
Frequency (n = 469) |
Percent (%) |
|
Sex of Patients |
|
|
|
Male |
198 |
42.2 |
|
Female |
271 |
57.8 |
|
Age group of Patients (Years) |
|
|
|
≤ 15 |
17 |
3.6 |
|
16 – 20 |
150 |
32 |
|
21 – 25 |
133 |
28.4 |
|
26 – 30 |
65 |
13.9 |
|
>30 |
104 |
22.2 |
|
Mean age: 25.21 ± 8.784 years |
|
|
|
Age Group at Diagnosis (Years) |
|
|
|
(n = 302) |
||
|
<1 |
22 |
7.3 |
|
1 – 3 |
105 |
34.8 |
|
4 – 6 |
85 |
28.1 |
|
7 – 9 |
34 |
11.3 |
|
10 – 12 |
16 |
5.3 |
|
>12 |
40 |
13.2 |
|
Steady State PCV (n = 153) |
|
|
|
15 – 19 |
19 |
12.4 |
|
20 – 24 |
82 |
53.6 |
|
25 – 29 |
42 |
27.5 |
|
>29 |
10 |
6.5 |
|
Mean PCV: 23.43 ± 3.622 |
|
|
|
History of Transfusion (n = 347) |
|
|
|
Yes |
246 |
70.9 |
|
No |
101 |
29.1 |
|
Only Child with HBSS in Household |
|
|
|
(n = 293) |
||
|
Yes |
214 |
73 |
|
No |
79 |
27 |
Table 1: Socio-demographic Characteristics and Disease History.
There were more females (271, 57.8%) than males (198, 42.2%) in the study; most of whom were within the age categories of 16 – 20 and 21 – 25. The mean age was 25.21 ± 8.784 years. The mean steady state PCV was 23.43 ± 3.622. Those who have had blood transfusion consisted 246 (70.9%) while households that have or have had only one HBSS child accounted for 214 (73.0%).
|
Variable |
Frequency |
Percent |
|
Multiple Response (n = 124) |
||
|
Complications |
|
|
|
Avascular Necrosis |
50 |
44.6 |
|
Chronic Leg Ulcer |
57 |
50.9 |
|
Osteomyelitis |
14 |
12.5 |
|
Osteo-Arthritis |
3 |
2.7 |
Table 2: Orthopedic complications.
Chronic leg ulcer and a vascular necrosis were the more common orthopedic complications, accounting for 50.9% and 44.6% of orthopedic complications among patients.
|
Variable |
Sex of Patients |
Fishers’ Exact |
|
|
(p-value) |
|||
|
Complications |
Male |
Female |
|
|
n (%) |
n (%) |
||
|
Avascular Necrosis |
19 (9.6) |
31 (11.4) |
0.549 |
|
Chronic Leg Ulcer |
23 (11.6) |
34 (12.5) |
0.777 |
|
Osteomyelitis |
3 (1.5) |
11 (4.1) |
0.168 |
|
Osteo-Arthritis |
2 (1.0) |
1 (0.4) |
0.576 |
Table 3: Association between Sex and Orthopedic Complications.
The association between sex and orthopedic complications were not statistically significant, as shown by Fishers’ Exact test.
|
Variable |
Age Group of Patients (Years) |
Fishers’ Exact |
|
|
Merged |
(p-value) |
||
|
Complications |
≤ 25 |
>25 |
|
|
n (%) |
n (%) |
||
|
Avascular Necrosis |
26 (8.7) |
24 (14.2) |
0.085 |
|
Chronic Leg Ulcer |
28 (9.3) |
29 (17.2) |
0.018 |
|
Osteomyelitis |
5 (1.7) |
9 (5.3) |
0.044 |
|
Osteo-Arthritis |
1 (0.3) |
2 (1.2) |
0.296 |
Table 4: Association between Age Group Orthopedic Complications.
Fishers’ Exact test shows a statistically significant association between orthopedic complications and age group of patients, this includes chronic leg ulcer and osteomyelitis, having p-values of 0.018 and 0.044.
Discussion
A wide range of the Nigerian population have been reported to have poor knowledge of sickle cell disease including secondary school students, [30-31] undergraduates, [32-33] local government workers, [34] and women of childbearing-age [35-37]. The fact that Sub-Sahara Africa has the highest prevalence of this abnormal hemoglobin disease (with Nigeria having the largest population of the patients), [38] did not change the experience of poor knowledge. The abnormality associated with the beta chain alteration (valine replaces glutamic acid in position six) is responsible for the path physiologic changes seen when the red cell sickles following exposure to triggers such as low altitudes, infections, extremes of temperature amongst others [27]. This change has considerably negative impact on the patients’ organs / systems including the bones and joints, irrespective of the patient’s sex. In this study, there were more females with orthopedic complications. This finding differs from the reports from Enugu and Lagos Nigeria where majority of the patients were males, [23-25] but share similarity with a South-South Nigeria study where female patients predominated [27]. Majority of our patients were in their young age (mean age was 25.21 ± 8.784 years), as seen in most other studies.
No statistically significant relationship was found between patients’ gender and orthopedic complications. Our finding is in agreement with another report from a Nigerian study where no relationship was found with gender [23]. However, a statistically significant relationship was found between the age group of these patients and orthopedic complications (Chronic leg ulcer /Osteomyelitis - p-values of 0.018 and 0.044 respectively), making our study finding different from that of Enugu Nigeria study [23]. The mean steady state packed cell volume of the patients was 23.43 ± 3.622. This value is close to the value of 24.46±4.76 reported in a Lagos Nigeria Study, [39] but lower than the value of 27.18 ± 5.35% from North Maharashtra in India [40]. However, the steady state packed cell volume in our study is higher than the value of 20.7 reported in a Zaria (Nigeria) study for SCA patients withChronic leg ulcer [41]. Majority (70.9%) of the households of these patients had only one child with HB SS, while the rest had more than one. This finding may vary depending on the society in question and the genotype of the parents.
Chronic leg ulcer was prevalent in about half (50.9%) of our patients, and a vascular necrosis in 44.6% of the patients, followed by Osteomyelitis. These findings highlight the significant burden of orthopedic complications in patients with SCA. A vascular necrosis of the femoral head, a condition characterized by the death of bone tissue due to poor blood supply, was observed in a considerable number of individuals. Chronic leg ulcers, which can significantly impact mobility and quality of life, were also prevalent. Osteomyelitis, a bone infection, was identified in a subset of the study population. The presence of osteoarthritis further emphasizes the long-term impact of SCA on joint health. Osteomyelitis was the commonest orthopedic complication of the disease as seen in Lagos some 12 years ago [25]. There were higher number of patients with chronic leg ulcer and a vascular necrosis than was reported in Lagos, [25] and relatively similar to the report outside Nigeria for osteonecrosis [42] However, a review article published in year 2015 reported vascular necrosis, osteomyelitis, septic arthritis, leg ulcer, etc. as the most common orthopedic complications of sickle cell anemia [23].
Study Limitations
The findings of this study were derived from a retrospectively collected data from medical records. It is therefore limited by the general demerits of this type of study.
Conclusion
Orthopedic complications are common in adults with Sickle Cell Anemia (SCA), and a vascular Necrosis of the Femoral head, Chronic leg ulcers, Osteomyelitis, and Osteoarthritis were the most frequently observed complications seen in Port Harcourt. These findings underscore the need for comprehensive management strategies and multidisciplinary care to minimize the impact of these complications on the quality of life of individuals with SCA.
Other Information
Ethical considerations: The approval of the Research Ethics Committee of the Rivers State University Teaching Hospital was obtained. This study involved only contact with medical records with no contact with the individual patients.
Source of Funding: The study was self-funded by the researchers.
Conflict of Interest: None declared.
References
-
Adewoyin AS. (2015) Management of sickle cell disease: a review for physician education in Nigeria (sub-saharan Africa). Anemia. 1-22.
-
Piel FB, Rees DC, DeBaun MR, Nnodu O, Ranque B, et al. (2023) Defining global strategies to improve outcomes in sickle cell disease: a Lancet Haematology Commission. Lancet Haematol. 10(8):E633-86.
-
Thomson AM, McHugh TA, Oron AP, Teply C, Lonberg N, et al. (2023) Global, regional, and national prevalence and mortality burden of sickle cell disease, 2000–2021: a systematic analysis from the Global Burden of Disease Study 2021. Lancet Haematol. 10(8):E585-99.
-
Amarapurkar P, Roberts L, Navarrete J, El Rassi F. (2022) Sickle cell disease and kidney. Adv Chronic Kidney Dis. 29(2):141-8.
-
Alakbarzade V, Maduakor C, Khan U, Khandanpour N, Rhodes E, et al. (2023) Cerebrovascular disease in sickle cell disease. BMJ Publishing Group Ltd. 91(1):131-8.
-
CAMPBELL EH. (1935) Acute abdominal pain in sickle cell anemia. Arch Surg. 31(4):607-21.
-
Martins RA, Soares RS, Vito FBD, Barbosa VdF, Silva SS, et al. (2017) Cholelithiasis and its complications in sickle cell disease in a university hospital. Rev Bras Hematol Hemoter. 39(1):28-31.
-
Ibinaiye PO, Babadoko AA, Yusuf R, Hassan AA. (2013) Renal complications of sickle cell anemia in Zaria, Nigeria: An ultrasonographic assessment. West Afri J Radiol. 20(1):19-22.
-
Vanderhave KL, Perkins CA, Scannell B, Brighton BK. (2018) Orthopedic manifestations of sickle cell disease. J Am Acad Orthop Surg. 26(3):94-101.
-
Cusano J, Curry EJ, Kingston KA, Klings E, Li X. (2019) Epidemiology and perioperative complications in patients with sickle cell disease after orthopaedic surgery: 26 Years' experience at a major academic center. J Am Acad Orthop Surg. 27(23):e1043-e51.
-
Kavanagh PL, Fasipe TA, Wun T. (2022) Sickle cell disease: a review. Jama. 328(1):57-68.
-
Nwadinigwe C, Anyaehie U, Ogbu D, Muoghalu O. (2011) Orthopaedic complications of sickle cell disease: a review. Nigerian Journal of Orthopaedics and Trauma. 10(2):81-88.
-
Koshy M, Weiner SJ, Miller ST, Sleeper LA, Vichinsky E, et al.(1995) Surgery and anesthesia in sickle cell disease. Cooperative Study of Sickle Cell Diseases. 86 (10):3676-84.
-
Buck J, Davies SC. (2005) Surgery in sickle cell disease. Hematology/Oncology Clinics. 19(5):897-902.
-
Adjepong KO, Otegbeye F, Adjepong YA. (2018) Perioperative management of sickle cell disease. Mediterr J Hematol Infect Dis. 10(1):e2018032.
-
Khurmi N, Gorlin A, Misra L. (2017) Perioperative considerations for patients with sickle cell disease: a narrative review. Can J Anesth. 64(8):860–69.
-
Walker I, Trompeter S, Howard J, Williams A, Bell R, et al. (2021) Guideline on the peri‐operative management of patients with sickle cell disease: Guideline from the Association of Anaesthetists. Anaesth. 76(6):805-17.
-
Shah N, Lipato T, Alvarez O, Delea T, Lonshteyn A, et al. (2022) Real-world effectiveness of voxelotor for treating sickle cell disease in the US: a large claims data analysis. Expert Rev hematol. 15(2):167-73.
-
Brown C, Idowu M, Drachtman R, Beaubrun A, Agodoa I, et al. (2023) Patient-Reported Experiences in Voxelotor-Treated Children and Adults with Sickle Cell Disease: A Semistructured Interview Study. BioMed Res Int. 7533111.
-
Howard J, Ataga KI, Brown RC, Achebe M, Nduba V, et al. (2021) Voxelotor in adolescents and adults with sickle cell disease (HOPE): long-term follow-up results of an international, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Haematol. 8(5):e323-e33.
-
Metcalf B, Chuang C, Dufu K, Patel MP, Silva-Garcia A, et al. (2017) Discovery of GBT440, an orally bioavailable R-state stabilizer of sickle cell hemoglobin. ACS Med Chem Lett. 8(3):321-26.
-
Oksenberg D, Dufu K, Patel MP, Chuang C, Li Z, et al. (2016) GBT 440 increases haemoglobin oxygen affinity, reduces sickling and prolongs RBC half‐life in a murine model of sickle cell disease. Br J Haematol. 175(1):141-53.
-
Chinawa J, Chukwu B, Ikefuna A, Emodi I. (2013) Musculoskeletal Complications Among Children with Sickle Cell Anemia Admitted in University of Nigeria Teaching Hospital Ituku‑Ozalla Enugu: A 58 Month Review. Ann Med Health Sci Res. 3(4):564-67.
-
Onyemaechi N, Enweani U, Maduka C. (2011) Musculoskeletal complications of sickle cell disease in Enugu, Nigeria. Nigerian Journal of Medicine. 20(4):456-561.
-
Balogun RA, Obalum DC, Giwa SO, Adekoya-Cole TO, Ogo CN, et al. (2010) Spectrum of musculo-skeletal disorders in sickle cell disease in Lagos, Nigeria. J Orthop Surg Res. 5:2.
-
Akinyoola AL, Adediran IA, Asaleye CM. (2007) Avascular necrosis of the femoral head in sickle cell disease in Nigeria: a retrospective study. Niger Postgrad Med J. 14(3):217-220.
-
Akaba K, Nwogoh B, Obanife H, Essien O, Epoke E. (2020) Prevalence of chronic complications in adult sickle cell anemia patients in a tertiary hospital in South-South Nigeria. Niger J Med. 29(4):665-69.
-
Yongu W, Elachi I, Mue D, Kortor J, Orkuma J, et al. (2018) Musculoskeletal Complications of Sickle Cell Anaemia and Their Management Approaches in Makurdi, Nigeria. Asian J Med Health. 9(3):1-8.
-
Madu AJ, Madu A, Umar G, Ibekwe K, Duru A,et al. (2014) Avascular necrosis in sickle cell (homozygous S) patients: Predictive clinical and laboratory indices. Niger J Clin Pract. 17(1):86-89.
-
Bazuaye G, Olayemi E. (2009) Knowledge and attitude of senior secondary school students in Benin City Nigeria to Sickle Cell Disease. World J Med Sci. 4(1):46-49.
-
Olakunle OS, Kenneth E, Olakekan AW, Adenike O-B. (2013) Knowledge and attitude of secondary school students in Jos, Nigeria on sickle cell disease. Pan Afr Med J. 15(1):127.
-
Hussaini M, Durbunde A, Jobbi Y, Muhammad I, Mansur A, et al.(2019) Assessment of experience, perception and attitude towards premarital sickle cell disease screening among students attending federal college of education, Kano, Nigeria. Niger Int J Res Rep Hematol. 2(1):1-12.
-
Alao O, Araoye M. (2009) Knowledge of sickle cell disease and haemoglobin electrophoresis: a survey of students of a tertiary institution. Niger J Med. 18(3):326-29.
-
Abioye-Kuteyi EA, Osakwe C, Oyegbade O, Bello I. (2009) Sickle cell knowledge, premarital screening and marital decisions among local government workers in Ile-Ife, Nigeria. Afr J Prim Health Care Fam Med. 1(1):1-5.
-
Otovwe A, Sunday U, Oghenenioborue Rume O, Awulo D. (2019) Knowledge and attitude of premarital genotype screening among women of child-bearing age in kumo-akko local government area of Gombe State Nigeria. Open J Public Health. 1(2):1006.
-
Babalola OA, Chen CS, Brown BJ, Cursio JF, Falusi AG, et al. (2019) Knowledge and health beliefs assessment of Sickle cell disease as a prelude to neonatal screening in Ibadan, Nigeria. J Glob Health Rep. 3:e2019062.
-
Agofure O, Danzaria M. (2020) Knowledge and attitude towards premarital genotype screening among women of child-bearing age in kumo akko local government area of Gombe State. Open J Med Res. 1(1):10-19.
-
Aliyu ZY, Kato GJ, Taylor IV J, Babadoko A, Mamman AI, et al. (2008) Sickle cell disease and pulmonary hypertension in Africa: a global perspective and review of epidemiology, pathophysiology, and management. Am J Hematol. 83(1):63-70.
-
Akinbami A, Dosunmu A, Adediran A, Oshinaike O, Phillip A, et al. (2012) Steady state hemoglobin concentration and packed cell volume in homozygous sickle cell disease patients in Lagos, Nigeria. Caspian J Intern Med. 3(2):405-409.
-
Jadhav A, Vaidya S, Bhagwat V, Ranade A, Vasaikar M. (2016) Haematological profile of adult sickle cell disease patients in North Maharashtra. Walawalkar International Medical Journal. 3(1):28-36.
-
Hassan A, Gayus DL, Abdulrasheed I, Umar MA, Ismail DL et al. (2014) Chronic leg ulcers in sickle cell disease patients in Zaria, Nigeria. Arch Intern Surg. 4(3):141-45.
-
Sathappan SS, Daniel Ginat M, Di Cesare PF. (2006) Multidisciplinary management of orthopedic patients with sickle cell disease. Orthopedics. 29(12):1094.
-
Vaishya R, Agarwal AK, Edomwonyi EO, Vijay V. (2015) Musculoskeletal manifestations of sickle cell disease: a review. Cureus. 7(10):e358.

