Mitochondria, Mood Lability, and Bone: mtSNPs’ Surprising Relationship to Mental Homeostasis
Elizabeth Mingo* and Chelsea Stephens
Howard University Department of Biology and Quadgrid Data Lab Research Group
*Corresponding author: Howard University Department of Biology and Quadgrid Data Lab Research Group
Citation: Mingo E and Stephens C. (2024) Mitochondria, Mood Lability, and Bone: mtSNPs’ Surprising Relationship to Mental Homeostasis. Adv Clin Med Res. 5(2):1-43.
Received: February 04, 2024 | Published: March 08, 2024
Copyright© 2024 genesis pub by Mingo E, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
DOI: https://doi.org/10.52793/ACMR.2024.5(2)-S1
Abstract
Mitochondrial DNA profiles comprise some of the most inclusive and broadly representative genomic databases publicly available, containing diverse haplogroups from all over the world; however, there is less emphasis on mutations' biochemical and neurological impact. Mitochondria’s function in calcium regulation is often cited, but few weave in its roles in immunity, bone homeostasis, cytokinesis, and apoptosis. While this approach is apt for increasing statistical significance, it can miss the bigger picture. Currently, there are enough associations—such as the effects of calcium dysregulation, the role of ROS in circadian rhythm determination, and cytokines’ interaction with mitochondria—to speculate on causality. This systematic review re-contextualizes previously reported haplotypes and single nucleotide polymorphisms (SNPs) in their biochemical environment, reports on potential systemic effects of altered mitochondria, explores common setbacks for studying bipolar disorders, and suggests new technologies that could ameliorate some of them using a novel graphic representation of each study’s findings.
Keywords
mtDNA; SNP; Mitochondria; Homeostasis; Bone homeostasis; Calcium; Calcium regulation; TNF-α; Cytokines; TFAM; P2X7R; ROS production; CACNA1C; RANKL; MCU; α-CaMKII; CAMK2II; IL-6; CRP; C-reactive protein; ROS; IL-1β; Mitochondrial morphology.
Introduction
Although humans’ mtDNA is uniformly circular, everyone differs in the number of mtDNA molecules per mitochondrion (copy number) [5,6], the exact haplotype of the mtDNA, the level of heteroplasmy (intra-individual mtDNA haplotype diversity) [7], and even the shape of their mitochondria [8].
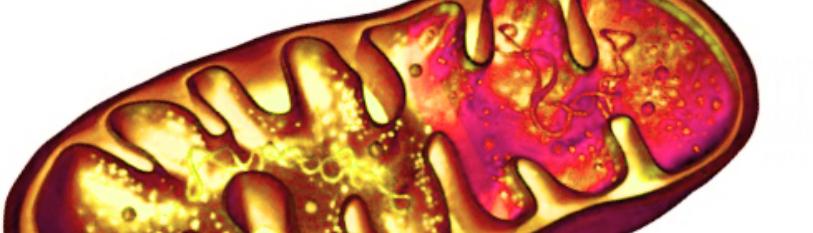
Such a varied structure suggests a multitude of functions, which proves correct. Mitochondria house the TCA cycle and the electron transport chain (ETC). Additionally, they engage in lipid metabolism, release ROS (signaling molecules on top of their damaging nature [9]), engage in calcium signaling [10,11], facilitate apoptosis [12], and regulate both nuclear and mitochondrial protein degradation [13].
This, together with mitochondria’s systemic roles in cytokinesis [14]], immunity [14-17], neurology [5] [6,18], and bone homeostasis [19,20], make it a versatile powerhouse within the body. Free-floating mitochondria have been found in both human and fetal bovine sera, expressing genes that regulate immune function [21]. However, this means that any downtick in utility has the potential to cause complex, messy disorders that do not fit nicely into any other box. Due to neurons’ steep energy demands, the brain is on the frontline of any metabolic disorder. This is seen clearly in altered mental statuses conferred by diabetic incidents [22] and the influence of eating disorders such as anorexia nervosa on confusion [23]. In other words, the symptoms of metabolic disorders bleed into psychiatry. Not everything that affects the brain occurs in the brain.
The etiologies of many mental illnesses, including bipolar, remain elusive. Bipolar is a group of mental disorders characterized by varying, prolonged, virtually unprompted periods of mania/hypomania, bipolar depression (as opposed to unipolar depression), and possibly mixed states. Psychosis and emotional blunting may occur throughout, and remission is known as euthymia. Euthymia is biochemically and mentally distinct from a normative mental state.
Bipolar disorders are subject to the kindling effect [24], meaning that each episode is more extreme than the last. It shares this phenomenon (as well as potential treatment with lamotrigine) with epilepsy.
Bipolar is the sixth leading cause of disability worldwide [33]. However, it overlaps with other disorders and is difficult to diagnose, with 31.9% of probands suffering for 13 years before finding the true diagnosis [34] [25]. This lack of identification is a huge problem; 25% of bipolar probands will attempt suicide in their lifetime, and 11% will succeed [34]. This combines with other factors to decrease probands’ lifespan by 11-20 years [35].
The list of comorbidities is lengthy, even putting aside other mental disorders: diabetes [26,27], low bone mass [28], decreases in visual motor perception [29], atrial fibrillation [30], asthma [31], dyslipidemia [36], hypertension [36], CVD [36], T. gondii infection [36], myocardial infarction [36], systemic lupus erythematosus [36], and temperature fluctuations [32]. When compared to healthy controls, bipolar probands present with activation changes in the thalamus [28], dorsolateral prefrontal cortex (DLPFC) [531*], hippocampus [28], and decreased volume in the anterior cingulate cortex [110*]. Many cytokines, such as TNF-α [39], vary significantly between states, as do serum and CSF calcium levels [40].
This prevalence, severity, and suicide risk all demand a convincing etiology—and mitochondria almost certainly play a role. Mitochondria interact with cytokines such as TNF-α [113], their count and morphology change in bipolar [114], and they are one of the main players in calcium signaling. Calcium homeostasis interacts with many of these comorbidities and symptoms [115]. However, this illness is complex. Solving the problem of its etiology will take a greater sample size than is reasonable from a singular study.
Although there are excellent reviews on bipolar disorders and mitochondrial physiology [41], there is no review of the utility of available databases. This review aims to integrate the physiology of mitochondria with the immune and skeletal system, explain salient existing database options, and clarify where they fall short for describing bipolar disorders.
Methods
PubMed was searched for the combinations of: “bipolar disorder,” “mtDNA,” "mitochondrial DNA,” “cytokine,” "bone," "calcium,” and "mitochondria” on 12-21-2023. These searches provided 580 results, or 521 unique articles, which were then appraised by the methods outlined in Fig. 1A. Only primary sources were included. Other reviews and meta-analyses were excluded to avoid the possibility of evaluating outdated or duplicate studies. Studies were considered “relevant” if they met the following criteria.
In epidemiological studies, the bipolar group had to be the test group/cohort of at least 100 subjects. Thus, a study on the effect of alcohol dependence on bipolar was excluded due to the confounding variable of alcohol dependence. If the study investigating bipolar was one of a few cohorts, and the bipolar sample met the qualifications, it was included. However, the results for non-bipolar mental disorders (such as ASD) were not reported. Studies needed to evaluate a characteristic of bipolar and not suggest a clinical course. If this epidemiological study was a genetic analysis, it had to specify a gene, not a haplogroup.
Mitochondrial haplotypes are broad categories, and results based on haplogroups are inconsistent. This does not mean that mtDNA is irrelevant—rather, smaller subgroups can influence the neurological risk of conditions such as Alzheimer ’s disease [42]. While there are no studies directly addressing subgroup analysis in bipolar disorder, it would certainly make sense of the discrepancies in the literature. To ensure even reporting, only specific mutations were considered.
Mouse studies’ requirements were similar: to have an appropriate strain and sample size. The appropriate sample size was met if the difference between the total animals and the total test groups was greater than 10.
In vitro studies needed slightly different inclusion/exclusion criteria. A list of comorbidities [43], medications, and biochemical markers associated with bipolar disorder were compiled. Relevant studies either investigated bipolar and one relevancy term or investigated three (or more) of the relevancy terms. The relevancy terms were as follows: childhood maltreatment/trauma, CVD, mitochondrial dysfunction, diabetes, dyslipidemia, senescence/aging, blood-brain barrier, metabolic syndrome, obesity, HPA disruption, bone mass, CKD, sleep deprivation, hippocampus, T. gondii, dentate gyrus, dorsolateral prefrontal cortex, prefrontal cortex, ROS/oxidative stress, mitochondrial copy number, mania/ hyperactivity (in mice), NF-κB, TNF-α, IL-6, IL-8, BRPF2, α-CaMKII, CRP, P2X7R, mitophagy, apoptosis, IL-1β, Lithium Lamotrigine, Valproate/valproic acid, Quetiapine, Olanzapine, Aripiprizole, Risperidone, any SSRIs, calcium, Complex 1, Complex 2, Polg1, LPS. iPSC studies claimed the correct significance, outlined in this review [44].
All relevant studies reported no author bias and had accurate abstracts. All were peer-reviewed.
Results from the relevant studies were tabulated in the supplementary table, which is the source for all the following figures to create ‘etiological fingerprints’ for each given variable—including comorbidities, cytokine elevations, ROS, cell cycle alterations, calcium alterations, and mitochondrial alterations. These were the columns of our table, with the exposure variables on the x-axis and our dependent variables on the y-axis. We then screened the following biometric databases for the qualities outlined in (Figure 1B) MITOMAP, MitBASE, MSeqDR, GnomA, PGC, and GWAS. The benefits and drawbacks of each were tabulated and compared to the literature review to estimate the efficacy of the available sources.
Results
Figure 1: The results of the literature and database review.
Diagnoses and Symptoms
Findings Map 1: A summary of dependent variables associated with bipolar and vetted symptoms of bipolar.
The finalists confirmed the existing notion that bipolar is an inflammatory disease. TNF-α, CRP, IL-1β, monocyte activators, and Complex I mutations all showed symptom profiles similar to bipolar. Both early and late onset bipolar were associated with mutations in Cytochrome B and Complex I, but the mutations differed. ND4 affected both phenotypes, whereas NDUFV2 was only associated with late onset [45] [46]. They also showed different epistasis—with late-onset preferring MGAM and early onset interacting with IL34 [46].
Although studies show consistent associations with TNF-α, IL-6, and IL-1β, these are dramatically affected by sample processing time, which may differ between collection sites [47]. While in vitro studies still support the involvement of these three cytokines, sample processing time remains a silent confounding variable for all epidemiological studies. The only cytokine that survived the correction was a decrease in IL-8. The effects of sample processing time on CRP were not tested. Even with this confounding variable, TNF-α, IL-6, CRP, and MCP-1 are all associated with the duration of bipolar and are differentially affected by depressive and manic states [48].
Medication
Findings Map 2: A summary of dependent variables associated with common medications for bipolar.
The etiological fingerprints of many medications prescribed for bipolar were also surveyed. Lithium and d-amphetamine were the most investigated drugs—lithium, because it is widely recognized as the gold standard for the treatment of bipolar (mania, in particular); d-amphetamine, because it can induce mania. These drugs are appealing proxies for euthymia/mania in vitro. No drug seemed to simulate mixed states, rapid cycling, or bipolar (as opposed to unipolar) depressive episodes.
All investigated drugs (except valproate) act on cytokines—especially IL-6, IL-1β, TNF-α, and IL-2. However, each has a unique profile. Lamotrigine is more effective against bipolar depression than mania and is exceptionally effective against rapid cycling [49]. Therefore, building a unique etiological fingerprint for each drug could illuminate subtle differences between mood disorders. Valproate, the drug with the least measured anti-inflammatory action, was the only drug found to independently increase fracture risk.
Lithium demonstrated anti-inflammatory properties, even in cerebral and cardiac ischemia [50]. It partially diminished the etiological fingerprint of bipolar—and lithium response correlated with an innate ability to ‘fill in the gaps.’ For example, one study found lithium increased cardiac IL-6; lithium-responsive rats showed a decreased concentration of IL-6 in the orbitofrontal cortex [51]. These are different tissues, but the larger pattern suggests the potential of a findings map—even when the findings from one study are unilluminating, it is easy to see that lithium responsivity protects against a potential inconsistency in lithium’s action. A findings map can identify intermittent problems quickly because they are all recorded in the same place.
Biochemical Findings
Findings Map 3: A summary of biochemical findings in bipolar.
In vitro studies highlighted LPS and PIC as the most common mechanisms of inducing cellular inflammation. Both produced etiological fingerprints similar to bipolar, but their intracellular effects differed. PIC goes through the TLR3 pathway, while LPS goes through the TLR4 pathway. The latter has been implicated in bipolar, whereas the former is seldom mentioned.
IL-6, ROS, TNF-α, and IL-1β formed the etiological fingerprint for LPS activation, which could all be normalized by inhibitors of the mitochondrial calcium uniporter (MCU) and antioxidants such as rice bran oil, açai extract, and palm oil. Some preliminary studies have even suggested that antioxidants such as CoQ10 aid the recovery of bipolar depression [52, confirming that this is not just an invitro phenomenon.
PIC elicited IL-6, TNF-α, IL-1β, and miscellaneous monocyte-activating factors. Maternal PIC exposure during pregnancy altered the glial density in bipolar-associated areas, such as the pyramidal neurons of the dorsal dentate gyrus, which interacted with adolescent social stress to create phenotypes such as gregariousness and hypermobility—both key symptoms of mania/hypomania.
Analogous Conditions
Findings Map 4: A summary of dependent variables associated with bipolar.
Certain comorbidities appeared in the course of the review. Diabetes looks dissimilar to bipolar; however, the study did not focus on the cytokine profile associated with the disease. It should be noted that Diabetes Mellitus Type II is associated with inflammation [36]. Sepsis was included due to the comorbidity of chronic infections, age was included because of the correlation with accelerated aging [53], and hypoxia was included as hypoxic injury may play a role in mood disorders [54].
One point of interest was that lithium was able to reverse the inflammation brought on by sepsis. This study was done on osteoblasts of normal C57BL/6 db/db mice. Even without a bipolar model, that data point suggests lithium’s anti-inflammatory mechanism is a direct effect of the drug and not a by-product of a purely psychological process.
Genetic and Transcriptive Anomalies
Findings Map 5: A summary of bipolar-associated genetic and transcription anomalies.
Genetic and transcriptive studies revealed important metabolic discrepancies—the most modified variables were ROS, locomotors activity, TNF-α, IL-6, and mitochondrial calcium. Disc1-Q31L interacted most with the elements of bipolar etiological fingerprint, followed closely by alterations in TFAM and CACNA1C. The MCU and CACNA1C showed the closest match for the etiological fingerprint of bipolar.
TFAM expression also affected many of bipolar important variables, but it had mixed effects. Sometimes, its cytokines would match bipolar' fingerprint; other times, it would deviate, but TFAM always affected bipolar' important elements. Differences in the expression and activity of MCU also created fingerprints similar to bipolar—MCU has a synergistic effect on the amount of ROS with CACNA1C. MCU and TFAM represent strong, under-researched links from mitochondria to neuropsychiatric disease.
Databases
| Database Criteria | MITOMAP | MitBASE | MSeqDR | GnomAD | PGC | GWAS Integrator |
| Type of data? | Genetic data | Genetic data | Genetic data | Genetic data | Genetic data | Genetic data |
| Large sample size? | No | No | No | Yes (up to 140,000 exomes and 15,000 whole genomes) | Yes (tens of thousands of individuals and controls) | Depends on trait or disease being studied |
| Genetic data (mtDNA and/or nDNA profiles?) | mtDNA, no focus on nDNA | mtDNA, no focus on nDNA | mtDNA, no focus on nDNA | nDNA, no focus on mtDNA | nDNA, no mtDNA | nDNA, no focus on mtDNA |
| Family History of Illness? | No family history of illness beyond any DIRECTLY related to mtDiseases | No | No family history of illness beyond any DIRECTLY related to mtDiseases | No, focuses on whole populations | Yes, collected for studies; however, detail varies among cases and studies | Yes, related to trait or disease being studied |
| Comorbidities? | Only those directly related to mtDiseases | Only those directly related to mtDiseases | Only those directly related to mtDiseases | No | Yes, but only for some studies | No |
| Number of Adverse Childhood Events? | No | No | No | No | Yes, but only for some studies | No |
| Longitudinal metabolic metrics labeled with mental state? | No | No | No | No | No | No |
| Open access? | Yes | Not accessible online | Basic features are available, some datasets have different access policies | Yes | Yes, however, some datasets are not available | Yes, however, specific datasets are not accessible |
| Forest plot generator? Statistical tools? | No | No | No | No forest plots - focuses on variant frequency | Offers extensive statistical tools but no forest plots | Offers extensive statistical tools but no forest plots |
Table 1: A summary of popular databases and their utility.
Several open-access databases provided excellent options for data mining. PGC approached the stringent qualifications, but one would have to combine resources to investigate the role of mitochondria. PGC meets the nDNA requirement (which must be there understand the role of molecules such as TFAM and the MCU) but omits mtDNA. MITOMAP is the leading open-access mtDNA database surveyed but still suffers from a small sato mple size. Depending on the study, utilizing multiple mtDNA databases may be advisable. None have the sort of longitudinal metabolic data required to capture the etiology of psychiatric disorders. None have automatic tools for generating forest plots. Although these open-access tools are extensive, more work is needed to investigate mitochondria’s implications in neuropsychiatric disorders.
Discussion
The literature on bipolar is mixed, and it is not without its problems; however, enough agreement exists between in vitro, in vivo, and epidemiological studies to suggest that the link is not purely from sample processing time. Each study suffers from disparate confounding variables, but they all converge on a set of culprits: elevations in TNF-α., IL-6, IL-1β, and ROS; expression differences in CACNA1C (CamKIIα), TFAM, and Disc1-Q31L; and comorbidities of diabetes and insomnia. Including the action of common medications particularly strengthens this analysis—serving almost as a negative control.
Each medication has a different etiological fingerprint. Valproate interacts less with cytokines than lamotrigine, lithium, or topiramate; however, it is the only drug associated with an independent increase in fracture risk. Given TNF-α’s role in bone resorption (through RANKL), RANKL’s action on Complex I through ESCIT [55], Complex I’s association with bipolar (Findings Map 1), and risperidone’s long-term metabolism shift from plasma to bone marrow (Findings Map 2): bone physiology is heavily implicated in bipolar. Other affected processes included circadian rhythms, autophagy, apoptosis, angiogenesis, collagen deposition, osteoblast/clast differentiation, calcium regulation, cell signaling, ROS, bacterial immune response, T cell activation, and glial activation.
Epidemiological Studies
One silent problem in the psychiatric epidemiological world is diagnosis. The cultural reluctance of patients to come forward, symptomatic overlap with other conditions, and the presence of comorbidities make it difficult to distinguish bipolar from conditions like borderline personality disorder. Some studies sidestep this by having multiple psychiatrists confirm each diagnosis; however, this is not an option in many situations.
One easy variable to check is the sex of the probands. Bipolar is a sexually dimorphic condition on many levels—including the regulation of cytokines [56], whether mutations such as rs1006737 are risk factors [57], and the risk of rapid cycling [58]. The risk contributed by rs1006737 is particularly illustrating: in women, it is protective; in men, it is a risk factor. Had that study neglected to split its group by sex, they would likely have found no significant change. Many studies that found no significance in genetic or cytokine data did not split based on sex.
Finally, a large number of studies initially surveyed were inadequately controlled. The control group should exceed the test group, and it is ideal to use multiple controls if possible. Many studies that met the sample size requirement had disproportionately small control groups and thus were excluded.
Mouse Studies
The statistical problems found in epidemiological studies extend to mouse studies. Perhaps because most mouse studies represent a proof of concept, statistical rigor is lacking. Some studies were excluded because they neglected to include the strain and age of their rodents. Other excluded studies were as small as three mice per group, yet they tried to suggest an effect on an entirely different species. While it is essential to minimize waste of life and resources, there is a lack of standard statistical practices [59]—or, if they do follow statistical best practices, they were not reported in the methods sections. While consulting a statistician during the study design would be ideal, [59] provides excellent, open-access statistical resources for those interested in animal studies.
In vitro Studies
In vitro studies have their problems as well. iPSC studies fail to outrun statistical problems. Each cell line is derived from one individual, making it, at its root, a sample size of one. Many studies surveyed derived 3-5 iPSC lines (due to the difficulty of the procedure)—which is an incredible model, but it is not generalizable to the general public unless it is 1) an isogenic pair study, 2) a multiple isogenic pair study or 3) meets the minimum sample size for an epidemiological study [44]. No iPSC studies survived these criteria.
As for the rest of the cell cultures, one detail stood out: the 1% mix of penicillin/streptomycin used to prevent bacterial contamination. Many antibiotics, including penicillin and streptomycin [60], are known to cause mitochondrial dysfunction and ROS overproduction. This puts cybrid/cell culture studies on shaky ground; are the given mutations indicating a native change in ROS production, or are they simply showing a difference in the mitochondrial response to penicillin? This overlooked factor threatens the validity of every in vitro study surveyed.
Limitations
The present study also suffers from constraints. The etiological fingerprint of bipolar was composed solely from the studies reviewed. Biomarkers and symptoms are inevitably omitted from the supplementary table. For example, there was no dedicated search for disturbances in the HPA axis, so ‘cortisol levels’ were undervalued. Future reviews would develop an even more extensive findings map, increasing the value of bipolar’s “fingerprint.”
Applying the rigorous standards for iPSC studies eliminated human neurons, whereas many approved cell culture lines are derived from rat neurons. This is not ideal. Future studies would provide a better framework for weighing cell lines against each other.
Another note—although not necessarily a limitation—is heterogeneity in the tissues studied. The tissue type affects medication intake and the efficacy of modifying factors (Supplementary Findings Map). Even tiny differences across brain regions significantly affect how the cells secrete, respond to, and are exposed to any given independent variable. This diversity is necessary; however, it is important not to take studies as a blanket elevation, decrease, or non-significance of cytokines.
Improved studies would survey more databases, represent certainty in each study more clearly, and increase the scope of the review to include childhood trauma, neurotransmitter abnormalities, and HPA axis disturbances.
Looking Forward
There is a demand for innovative, well-controlled studies on bipolar in all areas mentioned. One promising area for epidemiological cytokine studies is the development of wearable, real-time cytokine measurement [61]. With the caveat of caution against generalizing cytokine levels between tissues, this is a badly needed, low-maintenance option that completely avoids the sample processing time issue while yielding a time-dependent cytokine fingerprint. Future studies should avoid combining the sample into a coed cohort.
Promising areas for further in vitro and in vivo research include the role of RANKL, ESCIT, TFAM, and the MCU on bipolar. The advent of CRISPR-based manipulation of mtDNA also allows for more targeted studies on Complex I and III. Above all, a sterile, antibiotic-free growth medium is badly needed.
As we move into the age of precision medicine, more attention must be paid to statistical validity and the intuitive presentation of continuous data. This means providing stellar databases with combined mtDNA and nDNA, simple tools for illustrating relative statistical validity, and basic features such as forest plot generators and force-directed graphs. Many filters should be available, and updating the database with more samples should be possible. Bipolar requires a dizzying scope of data and effort, making it the ideal disorder to target through open-source databases.
Acknowledgments
We thank the Quadgrid Data Lab Research Group for their support and input in this comprehensive review. Special thanks to Fatimah Jackson for her meticulous guidance, and to Javan Carter for fielding statistical questions.
Funding
Publication of this comprehensive review was supported by a small grant from QuadGrid Data Lab and from the Division of Engagement and Outreach, All of Us Research Program, National Institutes of Health under award number 1OT20D028395-01.
References
- Cavalier-Smith T. (2006) Origin of mitochondria by intracellular enslavement of a photosynthetic purple bacterium. Proc Biol Sci. 273(1596):1943-52.
- Cheng X, Ivessa AS. (2010) The migration of mitochondrial DNA fragments to the nucleus affects the chronological aging process of Saccharomyces cerevisiae. Aging Cell. 9(5):919-23.
- Kolesnikov AA, Gerasimov ES. (2012) Diversity of mitochondrial genome organization. Biochemistry. 77(13):1424–35.
- Karnkowska A, Vacek V, Zubáčová Z, Treitli SC, Petrželková R, et al. (2016) A eukaryote without a mitochondrial organelle. Curr Biol. 26(10):1274–84.
- Filograna R, Mennuni M, Alsina D, Larsson G. (2021) Mitochondrial DNA copy number in human disease: The more the better? Febs Lett. 595(8):976-1002.
- Grady JP, Murphy JL, Blakely EL, Haller RG, Taylor RW, et al. (2014) Accurate Measurement of Mitochondrial DNA Deletion Level and Copy Number Differences in Human Skeletal Muscle. PLOS ONE. 9(12):e114462.
- https://www.sciencedirect.com/book/9780128179277/goodmans-medical-cell-biology#book-description
- Cataldo AM, McPhie DL, Lange NT, Punzell S, Elmiligy S, et al. (2010) Abnormalities in Mitochondrial Structure in Cells from Patients with Bipolar Disorder. Am J Pathol. 177(2): 575-85.
- Garbarino S, Lanteri P, Bragazzi NL, Magnavita N, Scoditti E. (2021) Role of sleep deprivation in immune-related disease risk and outcomes. Comm Biol. 4(1):1-17.
- Rizzuto R. De Stefani D, Raffaello A, Mammucari C. (2012) Mitochondria as sensors and regulators of calcium signaling. Nat Rev Mol Cell Biol. 13(9):566-78.
- Moreau B, Nelson C, Parekh AB. (2006) Biphasic regulation of mitochondrial ca2+ uptake by cytosolic ca2+ concentration. Curr Biol. 16(16):1672–77.
- Ermak G, Davies KJ. (2002) Calcium and oxidative stress: From cell signaling to cell death. Mol Immunol. 38(10):713-21.
- Adzic M, Brkic Z, Bulajic S, Mitic M, Radojcic MB. (2016) Antidepressant Action on Mitochondrial Dysfunction in Psychiatric Disorders. Drug Dev Res. 77(7):400-406.
- Fang Q, Marié IJ, Giddings EL, Fortner KA, Yang R, et al. (2021) IL-6 enhances CD4 cell motility by sustaining mitochondrial Ca2+ through the noncanonical STAT3 pathway. Proc Natl Acad Sci U S A. 118(37): e2103444118.
- Vattemi G, Marini M, Ferreri NR, Hao S, Malatesta M, et al. (2013) Overexpression of TNF-α in mitochondrial diseases caused by mutations in mtDNA: Evidence for signaling through its receptors on mitochondria. Free Radic Biol Med. 63:108-14.
- Rackov G, Tavakoli Zaniani P, Shokri R, Monserrat J, Balomenos D. (2022) Mitochondrial reactive oxygen is critical for IL-12/IL-18-induced IFN-γ production by CD4+ T cells and is regulated by Fas/FasL signaling. Cell Death Dis. 13(6):1-14.
- Mills EL, Kelly B, J, L. A. (2017) Mitochondria are the powerhouses of immunity. Nat Immunol. 18(5):488-98.
- Norat P, Soldozy S, Sokolowski JD, Gorick CM, Kumar JS, et al. (2020) Mitochondrial dysfunction in neurological disorders: Exploring mitochondrial transplantation. Npj Regen Med. 5(1):1-9.
- Kalani A, Kamat PK, Voor MJ, Tyagi SC, Tyagi N. (2014) Mitochondrial epigenetics in bone remodeling during hyperhomocysteinemia. Mol Cell Biochem. 395(0):89–98.
- Zheng CX, Sui BD, Qiu XY, Hu CH, Jin Y. (2020) Mitochondrial regulation of stem cells in bone homeostasis. Trends in Mol Med. 26(1):89–104.
- Song X, Hu W, Yu H, Wang H, Zhao Y, et al. (2020) Existence of Circulating Mitochondria in Human and Animal Peripheral Blood. Int J Mol Sci. 21(6):2122.
- Nyenwe EA, Razavi LN, Kitabchi AE, Khan AN, Wan JY. (2010) Acidosis: The Prime Determinant of Depressed Sensorium in Diabetic Ketoacidosis. Diabetes Care. 33(8):1837-39.
- Brodrick B, Jacobs M, McAdams C. (2020) Psychosis in Anorexia Nervosa: A Case Report and Review of the Literature. Psychosomatics. 61(2):181-87.
- Weiss RB, Stange JP, Boland EM, Black SK, LaBelle DR, et al. (2015) Kindling of Life Stress in Bipolar Disorder: Comparison of Sensitization and Autonomy Models. J Abnorm Psychol. 124(1):4-16.
- Lublóy Á, Keresztúri JL, Németh A, Mihalicza P. (2020) Exploring factors of diagnostic delay for patients with bipolar disorder: a population-based cohort study. BMC Psychiatry. 20(1):75
- Charles EF, Lambert CG, Kerner B. (2016) Bipolar disorder and diabetes mellitus: Evidence for disease-modifying effects and treatment implications. Int J Bipolar Disord. 4:13.
- Breznoscakova D, Pallayova M. (2022) Bipolar disorder and type 2 diabetes mellitus: A bidirectional relationship. Eur J Psychiatry. 36(3):152–62.
- Li S, Qui Y, Teng Z, Chen J, Kang D, et al. (2020) Association Between Bipolar Disorder and Low Bone Mass: A Cross-Sectional Study with Newly Diagnosed, Drug-Naïve Patients. Front Psychiatry. 11:530.
- Brenner CA, Hetrick WP. (2014) Disturbances of visual motion perception in bipolar disorder. Bipolar Disord. 16(4):354-65.
- Chung P, Lin J. (2014) The Connection between Cardiac and Mental Disorder: Atrial Fibrillation in Patients with Psychiatric Disorder. Acta Cardiologica Sinica. 30(1):53-55.
- Wu K, Wang Y, Chen W, Lin Y, Wu K, et al. (2016) Significantly Higher Prevalence Rate of Asthma and Bipolar Disorder Co-Morbidity: A Meta-Analysis and Review Under PRISMA Guidelines. Medicine. 95(13):e3217.
- Pflug B, Johnsson A, Ekse AT. (1981) Manic-depressive states and daily temperature. Acta Psychiatr Scand. 63(3):277-89.
- Colombo C, Fossati A, Colom F. (2012) Bipolar disorder. Depression Research and Treatment. 1–2.
- Hilty DM, Leamon MH, Lim RF, Kelly RH, Hales RE. (2006) A Review of Bipolar Disorder in Adults. Psychiatry (Edgmont). 3(9):43-55.
- Kessing LV, Vradi E, Andersen PK. (2015) Life expectancy in bipolar disorder. Bipolar Disord. 17(5):543-48.
- Rosenblat JD, McIntyre RS. (2017) Bipolar disorder and Immune Dysfunction: Epidemiological Findings, Proposed Pathophysiology and Clinical Implications. Brain Sci. 7(11):144.
- Townsend J, Bookheimer SY, Foland LC, Sugar CA, Altshuler LL. (2010) FMRI abnormalities in dorsolateral prefrontal cortex during a working memory task in manic, euthymic and depressed bipolar subjects. Psychiatry Res. 182(1):22-9.
- Clark L, Sahakian BJ. (2008) Cognitive neuroscience and brain imaging in bipolar disorder. Dialogues Clin Neurosci. 10(2):153-65.
- Benedetti F, Aggio V, Pratesi ML, Greco G, Furlan R. (2020) Neuroinflammation in Bipolar Depression. Front Psychiatry. 11:71.
- Harrison PJ, Hall N, Mould A, Al-Juffali N, Tunbridge EM. (2021) Cellular calcium in bipolar disorder: Systematic review and meta-analysis. Mol Psychiatry. 26(8):4106-16.
- Lam J, Xu B, Yeo L, Cheah S, et al. (2023) Mitochondria dysfunction and bipolar disorder: From pathology to therapy. IBRO Neurosci Rep. 14:407-18.
- Liu H, Zhang Y, Zhao H, Du Y, Liu X, et al. (2021) The heterogeneity among subgroups of haplogroup J influencing Alzheimer’s disease risk. J Adv Res. 33:117-26.
- Lee Y, Mansur RB, Brietzke E, Kapogiannis D, Delgado-Peraza F, et al. (2021) Peripheral inflammatory biomarkers define biotypes of bipolar depression. Mol Psychiatry. 26(7):3395-06.
- Brunner JW, Lammertse HC, Van Berkel AA, Koopmans F, Li KW, et al. (2023) Power and optimal study design in iPSC-based brain disease modelling. Mol Psychiatry. 28(4):1545-56.
- Zhang J, Li X, Wang Y, Ji J, Yang F, et al. (2009) Association study on the mitochondrial gene NDUFV2 and bipolar disorder in the Chinese Han population. J Neural Transm (Vienna). 116(3):357-61.
- Ryu E, Nassan M, Jenkins GD, Armasu SM, Andreazza A, McElroy SL, Vawter MP, Frye MA, Biernacka JM. (2018) A Genome-Wide Search for Bipolar Disorder Risk Loci Modified by Mitochondrial Genome Variation. Mol Neuropsychiatry. 3(3):125-134.
- Pan AY, Ryu E, Geske JR, Zhou XY, McElroy SL, et al. (2020) The impact of sample processing on inflammatory markers in serum: Lessons learned. World J Biol Psychiatry. 21(3):230-37.
- Bai YM, Su TP, Tsai SJ, Wen-Fei C, Li CT, et al. (2014) Comparison of inflammatory cytokine levels among type I/type II and manic/hypomanic/euthymic/depressive states of bipolar disorder. J Affect Disord. 166:187-92.
- Bowden CL, Calabrese JR, McElroy SL, Rhodes LJ, Keck Jr PE, et al. (1999) The efficacy of lamotrigine in rapid cycling and non–rapid cycling patients with bipolar disorder. Biol Psychiatry. 45(8):953–58.
- Zhang L, An LT, Qiu Y, Shan XX, Zhao WL, et al. (2019) Effects of Aspirin in Rats with Ouabain Intracerebral Treatment-Possible Involvement of Inflammatory Modulation? Front Psychiatry. 10:497.
- Adams WK, Levesque DL, Cocker PJ, Kaur S, Bodnar TS, et al. (2020) Decreased motor impulsivity following chronic lithium treatment in male rats is associated with reduced levels of pro-inflammatory cytokines in the orbitofrontal cortex. Brain Behav Immun. 89:339-49.
- Mehrpooya M, Yasrebifar F, Haghighi M, Mohammadi Y, Jahangard L. (2018) Evaluating the effect of coenzyme Q10 augmentation on treatment of bipolar depression. J Clin Psychopharmacol. 38(5):460–66.
- Yang F, Barbosa IG, Vieira EL, Bauer ME, Rocha NP, et al. (2018) Further Evidence of Accelerated Aging in Bipolar Disorder: Focus on GDF-15. Transl Neurosci. 9:17-21.
- Zhao F, Yang J, Cui R. (2017) Effect of Hypoxic Injury in Mood Disorder. Neural Plast. 6986983.
- Marques-Carvalho A, Sardão VA, Kim HN, Almeida M. (2023) ECSIT is essential for RANKL-induced stimulation of mitochondria in osteoclasts and a target for the anti-osteoclastogenic effects of estrogens. Front Endocrinol (Lausanne). 14:1110369.
- Keshavarzi A, Eftekharian MM, Komaki A, Omrani MD, Kholghi Oskooei V, et al. (2019) Sexual dimorphism in up-regulation of suppressors of cytokine signaling genes in patients with bipolar disorder. BMC Psychiatry. 19(1):402.
- Strohmaier J, Amelang M, Hothorn LA, Witt SH, Nieratschker V, et al. (2013) The psychiatric vulnerability gene CACNA1C and its sex-specific relationship with personality traits, resilience factors and depressive symptoms in the general population. Mol Psychiatry. 18(5): 607-13.
- Lee S, Tsang A, Kessler RC, Jin R, Sampson N, et al. (2010) Rapid-cycling bipolar disorder: Cross-national community study. Br J Psychiatry. 196(3):217-25.
- Charan J, Kantharia ND. (2013) How to calculate sample size in animal studies? J Pharmacol Pharmacother. 4(4):303-306.
- Kalghatgi S, Spina CS, Costello JC, Liesa M, Morones-Ramirez JR, et al. (2013) Bactericidal Antibiotics Induce Mitochondrial Dysfunction and Oxidative Damage in Mammalian Cells. Sci Transl Med. 5(192):192ra85.
- Xu J, Yang B, Kong J, Zhang Y, Fang X. (2023) Real-Time Monitoring and Early Warning of a Cytokine Storm In Vivo Using a Wearable Noninvasive Skin Microneedle Patch. Adv Healthc Mater. 12(18):2203133.
- Abu-Rish EY, Dahabiyeh LA, Bustanji Y, Mohamed YS, Browning MJ. (2018) Effect of lamotrigine on in vivo and in vitro cytokine secretion in murine model of inflammation. J Neuroimmunol. 322:36-45.
- Ahmed D, Roy D, Jaworski A, Edwards A, Abizaid A, et al. (2019) Differential remodeling of the electron transport chain is required to support TLR3 and TLR4 signaling and cytokine production in macrophages. Sci Rep. 9(1):18801.
- Choi EM. (2012) Regulation of intracellular Ca (2+) by reactive oxygen species in osteoblasts treated with antimycin A. J Appl Toxicol. 32(2):118-25.
- Albayrak A, Halici Z, Polat B, Karakus E, Cadirci E, et al. (2013) Protective effects of lithium: a new look at an old drug with potential antioxidative and anti-inflammatory effects in an animal model of sepsis. Int Immunopharmacol. 16(1):35-40.
- Barbisan F, Azzolin VF, Teixeira CF, Mastella MH, Ribeiro EE, et al. (2017) Xanthine-Catechin Mixture Enhances Lithium-Induced Anti-Inflammatory Response in Activated Macrophages In Vitro. Biomed Res Int. 4151594.
- Castaño Barrios L, Da Silva Pinheiro AP, Gibaldi D, Silva AA, Machado Rodrigues E Silva P, et al. (2021) Behavioral alterations in long-term Toxoplasma gondii infection of C57BL/6 mice are associated with neuroinflammation and disruption of the blood brain barrier. PLoS One. 16(10):e0258199.
- Cui Z, Meng X, Zhuang S, Liu Z, Zhou F, et al. (2020) Schizophrenia, Bipolar Disorder, and Alzheimer's Disease are not Causal Factors of Bone Mineral Density: A Mendelian Randomization Analysis. Calcif Tissue Int. 106(2):131-46.
- Davizon-Castillo P, McMahon B, Aguila S, Bark D, Ashworth K, et al. (2019) TNF-α-driven inflammation and mitochondrial dysfunction define the platelet hyperreactivity of aging. Blood. 134(9):727-40.
- de Souza DV, Pappis L, Bandeira TT, Sangoi GG, Fontana T, et al. (2022) Açaí (Euterpe oleracea) presents anti-neuroinflammatory capacity in LPS-activated microglia cells. Nutr Neurosci. 25(6):1188-99.
- Desdín-Micó G, Soto-Heredero G, Aranda JF, Oller J, Carrasco E, et al. (2020) T cells with dysfunctional mitochondria induce multimorbidity and premature senescence. Science. 368(6497):1371-76.
- Faustmann TJ, Corvace F, Faustmann PM, Ismail FS. (2020) Effects of Lamotrigine and Topiramate on Glial Properties in an Astrocyte-Microglia Co-Culture Model of Inflammation. Int J Neuropsychopharmacol. 25(3):185-96.
- Gevorgyan MM, Zhanaeva SY, Alperina EL, Lipina TV, Idova GV. (2020) The composition of peripheral immunocompetent cell subpopulations and cytokine content in the brain structures of mutant Disc1-Q31L mice. Vavilovskii Zhurnal Genet Selektsii. 24(7):770-76.
- Giovanoli S, Weber-Stadlbauer U, Schedlowski M, Meyer U, Engler H. (2016) Prenatal immune activation causes hippocampal synaptic deficits in the absence of overt microglia anomalies. Brain Behav Immun. 55:25-38.
- Gold PW, Pavlatou MG, Michelson D, Mouro CM, Kling MAet al. (2015) Chronic administration of anticonvulsants but not antidepressants impair bone strength: clinical implications. Transl Psychiatry. 5(6): e576.
- Gubert C, Andrejew R, Figueiro F, Bergamin L, Kapczinski F, et al. (2021) Lithium-induced neuroprotective activity in neuronal and microglial cells: A purinergic perspective. Psychiatry Res. 295:113562.
- Guerrin CGJ, Prasad K, Vazquez-Matias DA, Zheng J, Franquesa-Mullerat M, et al. (2023) Prenatal infection and adolescent social adversity affect microglia, synaptic density, and behavior in male rats. Neurobiol Stress. 27:100580.
- Hoseth EZ, Krull F, Dieset I, Mørch RH, Hope S, et al. (2018) Exploring the Wnt signaling pathway in schizophrenia and bipolar disorder. Transl Psychiatry. 8(1):55.
- Hu XF, Wang L, Lu YZ, Xiang G, Wu ZX, et al. (2017) Adiponectin improves the osteointegration of titanium implant under diabetic conditions by reversing mitochondrial dysfunction via the AMPK pathway in vivo and in vitro. Acta Biomater. 61:233-48.
- Jiang M, Yan W, Li X, Zhao L, Lu T, et al. (2023) Calcium Homeostasis and Psychiatric Disorders: A Mendelian Randomization Study. Nutrients. 15(18):4051.
- Köhler-Forsberg O, Rohde C, Nierenberg AA, Østergaard SD. (2022) Association of Lithium Treatment with the Risk of Osteoporosis in Patients With Bipolar Disorder. JAMA Psychiatry. 79(5):454-63.
- Kuhny M, Hochdörfer T, Ayata CK, Idzko M, Huber M. (2014) CD39 is a negative regulator of P2X7-mediated inflammatory cell death in mast cells. Cell Commun Signal. 12:40.
- Lee GH, Hwang JD, Choi JY, Park HJ, Cho JY, et al. (2011) An acidic pH environment increases cell death and pro-inflammatory cytokine release in osteoblasts: the involvement of BAX inhibitor-1. Int J Biochem Cell Biol. 43(9):1305-17.
- Lee S, Yu S, Park HJ, Jung J, Go GW, et al. (2019) Rice bran oil ameliorates inflammatory responses by enhancing mitochondrial respiration in murine macrophages. PLoS One. 14(10): e0222857.
- Lei X, Tan G, Wang Y, Chen L, Cao Y, et al. (2023) Mitochondrial Calcium Nanoregulators Reverse the Macrophage Proinflammatory Phenotype Through Restoring Mitochondrial Calcium Homeostasis for the Treatment of Osteoarthritis. Int J Nanomedicine. 18:1469-89.
- Li N, Zhang X, Dong H, Zhang S, Sun J, et al. (2016) Lithium Ameliorates LPS-Induced Astrocytes Activation Partly via Inhibition of Toll-Like Receptor 4 Expression. Cell Physiol Biochem. 38(2):714-25.
- Li S, Qiu Y, Teng Z, Xu B, Tang H, et al. (2022) Research on biochemical indexes of bone metabolism in bipolar disorder: A cross-sectional study with newly diagnosed, drug-naïve patients. J Psychiatr Res. 151:197-204.
- Liu X, Li X, Zhu W, Zhang Y, Hong Y, et al. (2020) Exosomes from mesenchymal stem cells overexpressing MIF enhance myocardial repair. J Cell Physiol. 235(11):8010-22.
- May M, Beauchemin M, Vary C, Barlow D, Houseknecht KL. (2019) The antipsychotic medication, risperidone, causes global immunosuppression in healthy mice. PLoS One. 14(6): e0218937.
- Mezni A, Aoua H, Khazri O, Limam F, Aouani E. (2017) Lithium induced oxidative damage and inflammation in the rat's heart: Protective effect of grape seed and skin extract. Biomed Pharmacother. 95:1103-1111.
- Mezuk B, Morden NE, Ganoczy D, Post EP, Kilbourne AM. (2010) Anticonvulsant use, bipolar disorder, and risk of fracture among older adults in the Veterans Health Administration. Am J Geriatr Psychiatry. 18(3):245-55.
- Michels S, Ganjam GK, Martins H, Schratt GM, Wöhr M, et al. (2018) Downregulation of the psychiatric susceptibility gene Cacna1c promotes mitochondrial resilience to oxidative stress in neuronal cells. Cell Death Discov. 10(4):54.
- Motyl KJ, Beauchemin M, Barlow D, Le PT, Nagano K,et al. (2017) A novel role for dopamine signaling in the pathogenesis of bone loss from the atypical antipsychotic drug risperidone in female mice. Bone. 103:168-76.
- Nemeth CL, Tomlinson SN, Rosen M, O'Brien BM, Larraza O, et al. (2020) Neuronal ablation of mt-AspRS in mice induces immune pathway activation prior to severe and progressive cortical and behavioral disruption. Exp Neurol. 326:113164.
- Ohnishi T, Murata T, Watanabe A, Hida A, Ohba Het al. (2014) Defective craniofacial development and brain function in a mouse model for depletion of intracellular inositol synthesis. J Biol Chem. 289(15):10785-796.
- Pathak G, Agostino MJ, Bishara K, Capell WR, Fisher JL, et al. (2017) PDE11A negatively regulates lithium responsivity. Mol Psychiatry. 22(12):1714-24.
- Shvartsur R, Agam G, Uzzan S, Azab AN. (2022) Low-Dose Aspirin Augments the Anti-Inflammatory Effects of Low-Dose Lithium in Lipopolysaccharide-Treated Rats. Pharmaceutics. 14(5):901.
- Su JA, Cheng BH, Huang YC, Lee CP, Yang YH, et al. (2017) Bipolar disorder and the risk of fracture: A nationwide population-based cohort study. J Affect Disord. 218:246-52.
- Trebinska A, Högstrand K, Grandien A, Grzybowska EA, Fadeel B. (2014) Exploring the anti-apoptotic role of HAX-1 versus BCL-XL in cytokine-dependent bone marrow- derived cells from mice. FEBS Lett. 588(17): 2921-7. Valvassori SS, Resende WR, Varela RB, Arent CO, Gava FF, et al. (2018) The Effects of Histone Deacetylase Inhibition on the Levels of Cerebral Cytokines in an Animal Model of Mania Induced by Dextroamphetamine. Mol Neurobiol. 55(2):1430-39.
- Valvassori SS, Resende WR, Varela RB, Arent CO, Gava FF, et al. (2018) The Effects of Histone Deacetylase Inhibition on the Levels of Cerebral Cytokines in an Animal Model of Mania Induced by Dextroamphetamine. Mol Neurobiol. 55(2):1430-39.
- Valvassori SS, Tonin PT, Varela RB, Carvalho AF, Mariot E, et al. (2015) Lithium modulates the production of peripheral and cerebral cytokines in an animal model of mania induced by dextroamphetamine. Bipolar Disord. 17(5):507-17.
- Van der Veen DR, Laing EE, Bae SE, Johnston JD, Dijk DJ, et al. (2020) A Topological Cluster of Differentially Regulated Genes in Mice Lacking PER3. Front Mol Neurosci. 13:15.
- Vogel SZ, Schlickeiser S, Jürchott K, Akyuez L, Schumann J, et al. (2015) TCAIM decreases T cell priming capacity of dendritic cells by inhibiting TLR-induced Ca2+ influx and IL-2 production. J Immunol. 194(7):3136-46.
- Wang TY, Lee SY, Chen SL, Chang YH, Wang LJ, et al. (2022) Changes of immune-related factors in the blood of schizophrenia and bipolar disorder patients receiving monotherapy. Transl Psychiatry. 12(1):212.
- Woo K, Kim DH, Oh MH, Park HS, Choi CH. (2021) N-3-Hydroxy Dodecanoyl-DL-homoserine Lactone (OH-dDHL) Triggers Apoptosis of Bone Marrow-Derived Macrophages through the ER- and Mitochondria-Mediated Pathways. Int J Mol Sci. 22(14):7565.
- Xing C, Zhou Y, Xu H, Ding M, Zhang Y, et al. (2021) Sleep disturbance induces depressive behaviors and neuroinflammation by altering the circadian oscillations of clock genes in rats. Neurosci Res. 171:124-32.
- Yoshida K, Kirito K, Yongzhen H, Ozawa K, Kaushansky K, et al. (2008) Thrombopoietin (TPO) regulates HIF-1alpha levels through generation of mitochondrial reactive oxygen species. Int J Hematol. 88(1):43-51.
- Yu H, Xu Z, Qu G, Wang H, Lin L, et al. (2021) Hypoxic Preconditioning Enhances the Efficacy of Mesenchymal Stem Cells-Derived Conditioned Medium in Switching Microglia toward Anti-inflammatory Polarization in Ischemia/Reperfusion. Cell Mol Neurobiol. 41(3):505-24.
- Schmiderer L, Yudovich D, Oburoglu L, Hjort M, Larsson J. (2022) Site-specific CRISPR-based mitochondrial DNA manipulation is limited by gRNA import. Sci Rep. 12(1):1-9.
- Kim SA, Kim S, Park HJ. (2022) REM-Sleep Deprivation Induces Mitochondrial Biogenesis in the Rat Hippocampus. In Vivo. 36(4):1726-33.
- Valvassori SS, Resende WR, Dal-Pont G, Sangaletti-Pereira H, Gava FF, et al. (2017) Lithium ameliorates sleep deprivation-induced mania-like behavior, hypothalamic-pituitary-adrenal (HPA) axis alterations, oxidative stress and elevations of cytokine concentrations in the brain and serum of mice. Bipolar Disord. 19(4):246-58.
- Kazuno AA, Munakata K, Kato N, Kato T. (2008) Mitochondrial DNA-dependent effects of valproate on mitochondrial calcium levels in transmitochondrial cybrids. Int J Neuropsychopharmacol. 11(1):71-8.
- Kastl L, Sauer SW, Ruppert T, Beissbarth T, Becker MS, et al. (2013) TNF‐α mediates mitochondrial uncoupling and enhances ros‐dependent cell migration via NF‐ΚB activation in liver cells. FEBS Letters. 588(1):175–83.
- Clay H, Sillivan S, Konradi C. (2011) Mitochondrial Dysfunction and Pathology in Bipolar Disorder and Schizophrenia. Int J Dev Neurosci. 29(3):311.
- Kato T. (2017) Neurobiological basis of bipolar disorder: Mitochondrial dysfunction hypothesis and beyond. Schizophr Res. 187:62-66.
This article was originally published in a special issue entitled “Integrating Data Science into Clinical and Medical Research”, handled by Editor Dr. Fatimah Jackson.

