Malignant Transformation into Chondrosarcoma of a Retroperitoneal Residual Mass after Chemotherapy for a Testicular Seminoma (Germinal Cell Tumor)
Salah Berkane*, Mustapha Kheder, Hocine Sklab, Salim Belkherchi, Chemssedine Benkhelat and Youcef Mahmoudi
Head of Department of General and Oncologic Surgery, Bejaia Teaching Hospital, Algeria
*Corresponding author: Salah Berkane, Head of Department of General and Oncologic Surgery, Bejaia Teaching Hospital, Algeria
Citation: Berkane S, Kheder M, Sklab H, Belkherchi S, Benkhelat C, et al. (2020) Malignant Transformation into Chondrosarcoma of a Retroperitoneal Residual Mass after Chemotherapy for a Testicular Seminoma (Germinal Cell Tumor). Adv Clin Med Res. 1(2):1-5.
Received: June 12, 2020, | Published: July 17, 2020
Copyright© 2020 genesis pub by Berkane S, et al. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
Abstract
Introduction: The transformation into a chondrosarcoma of a residual nodal mass during the evolution of tumors of testicular germ cells treated with chemotherapy based on platinum salts is an exceptional possibility (Two cases reported in the literature). We report an observation illustrating this extremely rare situation.
Observation: It is a forty-eight year old man who was operated on for cancer of the right testicle. He underwent a right orchidectomy. The histological study of the operating room was in favor of a seminoma, classified stage I. Normal tumor markers. At three months postoperatively, a retroperitoneal mass of 3cm was detected on the computed tomography scan which did not stop increasing in size despite first and second line chemotherapy. Faced with the non-response to chemotherapy and the progression of the tumor, the patient was referred to us for surgical resection. The histological study of this tumor returned in favor of a well differentiated chondrosarcoma associated with residual ductal structures which are in favor of its germinal origin and which was confirmed by the immuno histochemical study. A Body-scan was requested but without being able to find the original site. Our patient also benefited from adjuvant radiation therapy to optimize local control of the disease in healthy margins. He is alive at fifty months with a good health postoperative and shows no local recurrence and the tumor markers are still negative. The diagnosis retained in our patient is a malignant transformation into chondrosarcoma of a ganglionic magma of a testicular seminoma after chemotherapy. In the literature, two similar cases have reported the discovery of chondrosarcoma following surgery on the lymph node residual mass of testicular cancer, including one case approving the germinal origin of chondrosarcoma by a cytogenetic study.
Conclusion: Our case and two reported literature cases, shows that transformation of retroperitoneal residual tumor of testicular seminoma into chondrosarcoma remains exceptional. Clinicians must precisely eliminate primitive chondrosarcoma with before retaining this diagnostic.
Introduction
The lymphnode metastases of testicular germ tumors are very chemosensitive and systemic chemotherapy had ameliorated the prognosis of the testicular tumors in ceit’s introduction in the eighty. Residual lymph nodes after chemotherapy need to be resected and in the majority of cases, histological exam found necrosis, teratoma or active tumor tissue. The malignant transformation into a chondrosarcoma of a residual nodal mass treated with chemotherapy based on platinum salts is an exceptional possibility (two cases reported in the literature to date). We report an observation illustrating this extremely rare situation.
Observation
This is a 48-year-old man who had surgery for right testicular cancer. He underwent a right orchidectomy. The histological study of the operating room was in favor of a seminoma, classified pT2N0M0. The tumor markers were normal. At three months postoperatively, a retroperitoneal mass suggestive of a metastatic lymph node of 3cm was detected on the CT scan. The patient received systemic chemotherapy based on three courses of Bleomycin, Epirubicin and Cisplatinum (BEP). The tumor mass continued to increase in size, going to six cm and after 9 cm despite the introduction of a second line of chemotherapy (four ourses of Docetaxel). This tumor had intimate contact with the inferior vena cava, the aorta, the right renal vein and the duodeno-pancreatic block. Faced with the non-response to chemotherapy and the progression of the tumor, the patient was referred to us for surgical resection. The latter was laborious and quite difficult at the same time. The tumor was well-defined, bumpy, stony and irregular in hardness. We only performed resection of this tumor because exploration of the retroperitoneal area was free from many suspected lymphadenopathy. The aftermath was simple. The histological study of this tumor returned in favor of a well-differentiated low-grade chondrosarcoma associated with residual ductal structures which suggest the very probable origin of metastatic ganglionic foci of seminoma and which was confirmed by an immunoassay histochemical. In view of these results, a Body Scan and x-rays of the bones of the whole body were requested, but without being able to find the original site in favor of a possible chondrosarcoma. Our patient benefited from adjuvant external radiotherapy (50 grays) in order to optimize the local control of the disease. The patient is alive at fifty postoperative months. He has no local recurrence and the tumor markers are still negative [1,2].
Discussion
Retroperitoneal sarcomas are rare tumors. They represent 0.5 to 1% of malignant tumors and 12% of soft tissue sarcomas [3-5].The sarcomas most encountered in the retroperitoneum are: Liposarcoma, Leiomyosarcoma, Malignant histiocytofibroma. Other histological forms are rare: Fibrosarcomas, Rhabdomyosarcomas, Synovialo sarcomas, Ewing's sarcomas, Malignant tumors of nervous origin and Chondrosarcoma. Retroperitoneal chondrosarcoma is rare [4,5]. It is of the mesenchymal or myxoid type [6]. In our patient, chondrosarcoma is well differentiated and is associated with residual ductal structures which are in favour of its germinal origin (immune-histochemistry in progress).
Generally, the residual mass after chemotherapy is of a nature: teratomatous (45%), necrosis (45%) and a still active tumor focus (10%) [7-10]. Malignant transformation of the residual masses occurs in a small proportion of patients with germ metastatic tumors treated with platinum salt chemotherapy. Chondrosarcoma has rarely been reported as a component of the second non-germ cell malignancy. The diagnosis retained in our patient is a malignant transformation into chondrosarcoma of lymphnode magma of a testicular germ cell tumor after chemotherapy.
The elements in favor of this hypothesis are:
- The appearance of the retroperitoneal tumor three months after the orchidectomy.
- The presence of residual canal structures associated with chondrosarcoma.
- The well differentiated histological type of chondrosarcoma.
- The immunohistochemical study which confirms the germinal origin of this retroperitoneal tumor.
- The absence of a primitive bone site.
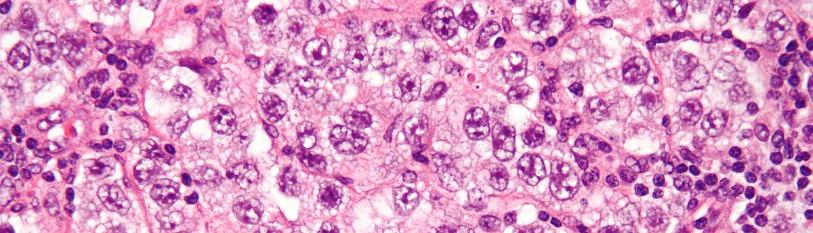
In the literature, two similar cases have reported the discovery of chondrosarcoma following lymphnode residual mass surgery for testicular cancer [1,2]. In one case, the germinal origin of chondrosarcoma was signed by a cytogenetic study [1]. In our patient, the diagnostic orientation in favour of a transformation is carried on the bundle of arguments cited above (Figure 1,2).
Figure 1: Macroscopic aspect of open tumor after resection.
Figure 2: Histological view; 2A: Well differentiated Chondosarcoma; 2B: Lonular Cartilaginous Into Fibrous Stroma; 2C: Fibro-Histiocitary Stroma; 2D: Residual Canal Structures.
Conclusion
The malignant transformation of a retroperitoneal mass into chondrosarcoma after chemotherapy is exceptional. The tumor was asymptomatic and diagnosed using a computed tomography scan. It is important to go to a more detailed histological study and carry out a search for a possible primary focus of chondrosarcoma before choosing that of the transformation of the tumor mass.
References
- Kirschner-Hermanns R, Fuzesi L, Sohn M, Jakse G. (1994) Therapy of primary testicular chondrosarcoma. Der Urologe. Ausg A. 33(6):517-20.
- Assimakopoulos SF, Koutras A, Ravazoula P, Makatsoris T, Petsas T, et al. (2006) A case of chondrosarcoma developing in a recurrent retroperitoneal mass after chemotherapy for testicular germ cell tumor. Urol Int. 77(1):86-8.
- Bonvalot S, Miceli R, Berselli M, Causeret S, Colombo C, et al. (2010) Aggressive surgery in retroperitoneal soft tissue sarcoma carried out at high-volume centres is safe and is associated with improved local control. Ann Surg Oncol. 17(6):1507-14.
- Avances J, Rigaud B, Bui P, Camparo S, Culine X, et al. (2010) Retroperitoneal Sarcoma: Contribution to the Repository CCAFU INCA.
- Jean-Dominique doublet and the members of the CCAFU kidney subcommittee. (2007) Retro-peritoneal sarcomas. 17(6):1153-5.
- PhAnract, G de Pinieux, B Tomeno. Orthopedic surgery service B, Hôpital Cochin, University of Paris V. Intraosseous chondrosarcomas.
- X Durand, J Rigaud, C Avancès, P Camparo, A Fléchon, et al. (2013) Recommendations in Onco-urology CCAFU:Germ cell testicular tumors. Members CCAFU Prog Urol. 23(S145-60):Suppl 2.
- Motzer RJ, Amsterdam A. (1998) Teratoma with malignant transformation: Various malignant histologies in men suffering from germinal tumors. Department of Medicine, Memorial Hospital, New York, USA. J Urol. 159(1):133-8.
- Sonneveld DJ, Sleijfer DT, Koops HS, Keemers Gels ME, Molenaar WM, et al. (1998) Mature teratoma identified after post chemotherapy surgery in patients with disseminated non-seminomatous testicular germ cell tumors: a plea for an aggressive surgical approach. CANCAR. 82(7):1343-51.
- Houlgatte (2008) Surgical management of retroperitoneal metastases of germinal tumors of testis. Department of Urology, Hôpital du Val de Grâce, Paris v France Progrès en Urologie. Suppl 7:S382-87.

