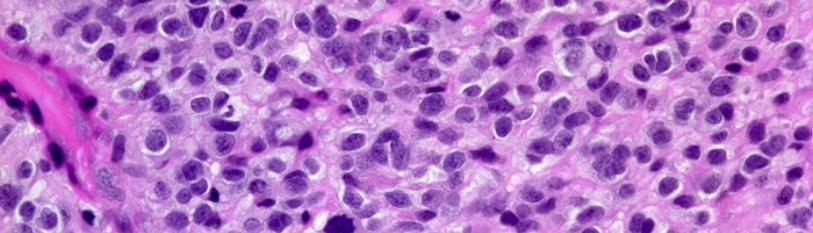
Systems of Active Immune Suppression as Integral Malignant Transformation in Infiltrating Glioma Cells
Lawrence M Agius*
Department of Pathology, Mater Dei Hospital, Tal Qroqq, University of Malta Medical School, MSIDA, Malta, Europe
*Corresponding author: Lawrence M Agius, Department of Pathology, Mater Dei Hospital, Tal Qroqq, University of Malta Medical School, MSIDA, Malta, Europe.
Citation: Agius LM. (2021) Systems of Active Immune Suppression as Integral Malignant Transformation in Infiltrating Glioma Cells. J Can Ther Res. 1(1):1-5.
Received: Aug 20, 2021 | Published: Aug 31, 2021
Copyright© 2021 Genesis Pub by Agius LM. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are properly credited.
DOI: https://doi.org/10.52793/JCTR.2021.1(1)-03
Abstract
Abstract
Immunologic tolerance to an infiltrating tumor cell bed is a very active process of suppression of the immune responsive mechanisms with a strong executive process of regressive adaptation of the adjacent infiltrated brain tissues. In such terms, constitutive realization of the malignant transformation process is a derived series of homeostatic mechanisms that adaptively come to adopt the significant aberrancy of a non-response on the part of systems of recognition and also of execution as borne out by the appraisal process of institutionalized pathways of attempted response to the infiltrating tumor cells.
Keywords
Active immune suppression, Tumor cell; Brain tissues; Glioblastoma
Introduction
The concentrated approach to the evolutionary development of primary malignant gliomas constitutes in reality an appreciation of events centered on cytokine production and delivery to the tumor cell bed, as primarily exemplified by resection cavity creation after subtotal surgical removal. Podoplanin-positive myeloid cells with transcriptional regulation of arginase-1 are one class of mediators of the glioma-modulated immune suppression [1]. Glioblastoma patients have a significant elevation of myeloid-derived suppressor cells in peripheral blood but not immunosuppressive Tregs [2]. The consequent delineation of injury to tumor cells is coupled to the presence of a blood brain barrier functionality and dysfunctionality. In such terms, the emergence of injury to neoplastic cells primary in the central nervous system (CNS) constitutes in itself the evolutionary hallmark of a series of immunologic attempts at potential eradication of the tumor lesion. Glioblastoma takeover involves soluble factors such as chemokine and cytokines, direct cell-cell contact, extracellular vesicles and micro-vesicles and connecting nanotubes and microtubes [3]. It is further to such concerns that the complete evolutionary nature of injury to tumor cells is beset by the delineation of a lesion that both infiltrates and proliferates in terms of a series of developmentally regressive changes.
Cytokines
It is a significant to view cytokine delivery systems as integral to the potential antitumor responses of the immune system in terms that abrogate the host’s environmental disposition to evade such immune responses. Toll-like receptor 2 enhances glioma immune evasion by down-regulating MHC Class II molecules in microglia [4]. It is within encompassed derivation of the neoplastic lesion that infiltration of the surrounding brain tissue dominates, in real terms, in the evolutionary adaptation of the CNS to a lesion that is suppressed immunologically. Activated dendritic cells, eosinophils, activated mast cells, monocytes and activated natural killer cells positively relate to prognosis of glioma patients whereas resting natural killer cell, CD8+ T cells, T follicular helper cells, gamma delta T cells and M0 macrophages negatively relate to prognosis [5]. The emergence of cell injury to a highly infiltrative and highly proliferative neoplastic lesion is beset by the spread phenomenon that diffusely compromises dynamics of turnover of immune cells within the CNS. Blocking myeloid-derived suppressor cells holds great promise for enhancing the efficacy of gene therapy-mediated immunotherapies for glioblastoma [6].
Constitutional Factors
Constitutive dynamics of recognition of tumor-associated antigens are de facto a system of failed retrieval within the immune system turnover and of the failed constitutive amplification of the antitumor immune response. Self-renewing cancer stem cells in glioblastoma possess expression of TLR4 that permits them to survive in spite of inflammatory signals [7].
In such terms, the further definition of injury to a primary tumor cell bed is hampered by the emergence of such features as the infiltrative proliferation inherent to malignant glioma evolutionary course. It is within systems for potent infiltrative definition that the primary malignant glioma both constitutes and further informs the significant suppression of an active immune response as primary consideration in primary tumor biology. The performance dynamics, as borne out by a system of primal infiltration, includes the delineation of an immune response that potentially can be activated in terms of antitumor potent response. In such terms, the outline phenomenon of infiltration of adjacent brain tissue is derivative process within the biologic evolution of the primary malignant glioma as relative to the proliferative biology of the glioma cells themselves.
In such terms, ongoing immune responsiveness is dynamic constitution as evolutionary substitution of normal homeostatic mechanisms as projected beyond the adjacent brain tissues. Several immunotherapies are being tested including inhibition of immune checkpoint regulators, antitumor vaccination from dendritic cell and tutor peptide components, adoptive transfer of supercharged and durable T lymphocytes, and the use of oncolytic viruses [8].
Conditioned Settings
The emerging conceptual settings of a primary neoplasm are derived dynamics of an injury that provokes proliferation of infiltrating cells in the first instance. Primarily infiltrating tumor cells are significantly dynamic in terms of resultant turnover processes of attempted renewal of the malignant transformation phenomenon. In such terms, ongoing derivative regression biologically and pathophysiologically is a failure of the responsiveness of the immune system that dynamically attempts at adaptation to altered homeostatic mechanisms. An essential turnover process lies at the heart of a concentrated effort to evade the immune responses within systems for further primary infiltrative behavior.
In such terms, ongoing redistribution of various metabolic substrates is subservient phenomenon within dynamic systems of primarily altered adaptation. It is further to such considerations that the overall homeostasis systems are adaptive to and also primarily inducive to a failed immunologic response to primarily infiltrative tumor cell beds. In addition to heterogeneous populations of tutor cells, glioma stem cells and other non tumor cells in the glioma microenvironment serve as critical regulators of tutor progression and recurrence [9]. Suppression of antitumor T cell immunity has been shown by the oncometabolite (R)-2-hydroxyglutarate [10].
Immune Response
Significant terms of attempted retrieval of the immune response to a malignant glioma is textual verification of an injury to glial cells that is portrayed and further projected as malignant transformation of a primarily infiltrating tumor cell population and of a series of further infiltrative phenomena. It is in such terms that the ongoing regression of a lesion is beset by a failure to recover an immune responsiveness within systems of dynamic turnover.
The performance attributes of such injury towards malignant transformation derive significance as terms of relative insufficiency of a primary and of a secondary immune response. It is clearly within such concept of integrative suppression of response that the derived phenomenon of re-constitutive biology both fails as homeostatic mechanism and also as derived turnover overactivity as projected in terms of performance dynamics. Mis-sense mutations in the active site of isocitrate dehydrogenase 1 (IDH1) biologically and also diagnostically distinguish low-grade gliomas and secondary glioblastomas from primary glioblastomas; mutant isocitrate dehydrogenase 1 expression drives gliomagenesis, mutant IDH1 itself is rapidly converted from driver to passenger [11]. In addition to R(-)-2-hydroxyglutarate, alterations in several other metabolites measured by magnetic resonance spectroscopy correlate with IDH1 mutation status [12].
Aberrant Immune Response
A primary aberrant immune response accounts for repression of an immune response that is homeostatically conditioned and reconditioned within systems of adaptive pathology of systems of pathogenesis of the malignant transformation process. There is increasing evidence that the dysregulated metabolic activity of neoplastic cells generates an immunosuppressive tutor microenvironment that orchestrates an impaired anti-timor immune response [13]. Novel combination treatments are warranted such as inhibition of histone deacetylases1/2 and of TRAP1 to induce synthetic lethality in glioblastomas [14]. In such terms, evolutionary derivation is both etiology and pathogenesis of an injury that recharacterizes the homeostatic mechanics of a proliferating tumor cell bed within systems of an aberrant immune response that in turn is responsible for the primarily infiltrative phenomenon. It is such setting that accounts for redefinition of tumor cell biology within confines of an abnormal reconditioning of a process of malignant transformation.
Concluding Remarks
Dynamics of attempted reconstitution are failure dynamics of a homeostatic conditioning within contextual reappraisal of a suppressed immune response to primarily infiltrating tumor cells of a malignant glioma lesion. In such terms, the derivative phenomenon of suppressive phenomena is integral to biology of responsiveness within systems of active recognition of tumor-associated and tumor-specific antigens. The cooperative evolutionary performance of integral dynamics further constitutes a system of immune tolerance as dictated by an aberrant series of immune responses. Significant emphasis is being made on targeting class II MHC transcription factors to either inhibit or stimulate the immune response in, especially, cell-based vaccines [15].
It is clearly the nature of aberrant responses that permissively condition such responses to active suppression as dictated by the infiltrative process of the tumor cells. It is further to such proposed dynamics that immune tolerance is a very active process of regressive adaptation within systems of both recognition and suppression of the immune system to the real immunologic identities of the infiltrative tumor cell bed.
References
- Eisemann T, Costa B, Peterziel H, Angel P. (2019) “Podoplanin positive myeloid cells promote glioma development by immune suppression” Front Oncol. 9:187.
- Alban TJ, Alvarado AG, Sorensen MD, Bayik D, Volovetz J, et al. (2018) “Global immune fingerprinting in glioblastoma patient peripheral blood reveals immune-suppression signatures associated with prognosis” JCI Insight. 3(21):e122264.
- Broekman ML, Maas SLN, Abels ER, Mempel TR, Krichevsky AM, et al. (2018) “Multidimensional communication in the micro environs of glioblastoma” Nat Rev Neural. 14(8):482-95.
- Qian J, Luo F, Yang J, Liu J, Liu R, et al. (2017) “TLR2 promotes glioma immune evasion by down regulating MHC Class II molecules in microglia” Cancer Immunol Res. 6(10):1220-33.
- Zhong QY, Fan EX, Feng GY, Chen QY, Gou XX, et al. (2019) “A gene expression-based study on immune cell subtypes and glioma prognosis” BMC Cancer. 19(1):1116.
- Kamran N, Kadiyala P, Saxena M, Candolfi M, Li Y, et al. (2017) “Immunosuppressive myeloid cells ‘blockade in glioma microenvironment enhances the efficacy of immune-stimulatory gene therapy” Mol Ther. 25(1):232-48.
- Alvarado AG, Thiagarajan PS, Mulkearns-Hubert EE, Silver DJ, Hale JS, et al. (2017) “Glioblastoma cancer stem cells evade innate immune suppression of self-renewal through reduced TLR4 expression” Cell Stem Cell. 20(4):450-61.
- Wilcox JA, Ramakrishna R, Magge R. (2018) “Immunotherapy in glioblastoma” World Neurosurg. 116:518-28.
- Ma Q, Long W, Xing C, Chu J, Luo M, et al. (2018) “Cancer Stem cells and immunosuppressive microenvironment in glioma” Front Immunol. 9:2924.
- Bunse L, Pusch S, Bunse T, Sahm F, Sanghvi K, et al. (2018) “Suppression of antitumor T cell immunity by the oncometabolite (R)-2-hydroxyglutarate” Nat Med. 24(8):1192-03.
- Johannessen TCA, Mukherjee J, Viswanath P, Ohba S, Ronen S, et al. (2016) “Rapid conversion of mutant IDH1 from driver to passenger in a model of human gliomagenesis” Mol Cancer Res. 14(10):965-83.
- Pope WB, Prins RM, Thomas MA, Nagarajan R, Yen KE, et al. (2012) “Non-invasive detection of 2-hydroxyglutarate and other metabolites in IDH1 mutant glioma patients using magnetic resonance spectroscopy” J Neurooncol. 107(1):197-205.
- Jiang Z, Hsu JL, Li Y, Hortobagyi GN, Hung MC. (2020) “Cancer cell metabolism bolsters immunotherapy resistance by promoting an immunosuppressive tumor microenvironment” Front Oncol. 10:1197.
- Nguyen TTT, Zhang Y, Shang E, Shu C, Quinzii CM, et al. (2020) “Inhibition of HDAC1/2 along with TRAP1 causes synthetic lethality in glioblastoma model systems” Cells. 9(7):1661.
- Radosevich M, Ono SJ. (2003) “Novel mechanisms of class II major histocompatibility complex gene regulation” Immunol Res. 27(1):85-106.

