Future plans of Treating a Case of Acquired Pure Red Cell Aplasia Secondary to Autoimmune Causes Resistant to Combination of Cyclosporine and Corticosteroid
Kulvinder Kochar Kaur1*, Gautam Allahbadia2 and Mandeep Singh3
1Centre for Human Reproduction, 721, GTB Nagar, Jalandhar, 144001 Punjab, India
2Ex-Rotunda, A Centre for Human Reproduction, Mumbai, India
3Consultant Neurologist, Swami Satyanand Hospital, Jalandhar, India
*Corresponding author: Kulvinder Kochar Kaur, Centre for Human Reproduction, 721, GTB Nagar, Jalandhar, Punjab, India.
Citation: Kaur KK, Allahbadia G, Singh M. (2020) Future plans of Treating a Case of Acquired Pure Red Cell Aplasia Secondary to Autoimmune Causes Resistant to Combination of Cyclosporine and Corticosteroid. Adv Clin Med Res. 1(1):1-9.
Received: April 24, 2020, | Published: May 10, 2020
Copyright© 2020 genesis pub by Kaur KK. CC BY-NC-ND 4.0 DEED. This is an open-access article distributedunder the terms of the Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International License.,This allows others distribute, remix, tweak, and build upon the work, even commercially, as long as they credit the authors for the original creation.
Abstract
Pure red cell aplasia (PRCA) is an orphan disease, and as such there are no rationally developed standard treatments. Most of the cases are idiopathic with a subset being antibody mediated. An overlap exists among idiopathic cases with those of T cell large granular lymphocytic leukemia, hypogamma globulinemia as well a slow grade lymphoma. Here we report a case of acquired Pure red cell aplasia (aPRCA), who did not attain Complete remission (CR) with calcineurin inhibitor (cyclosporine A) along with prednisone 50 mg od, being associated with 2 autoimmune disorders like systemic lupus erythemzatosus (SLE) with endometriomas and has now displayed partial remission (PR) with a combination of prednisolone 50mg with anabolic steroid danazol 200mg bd for 4 months along with metoclopramide 10mg od and is being continued on same therapy for minimum of 18 months for getting a CR as did another case of SLE as well as a case of anky losing spondylitis.
Keywords
APRCA; Cyclosporine A; Prednisone; Danazol; Autoimmune disorders
Introduction
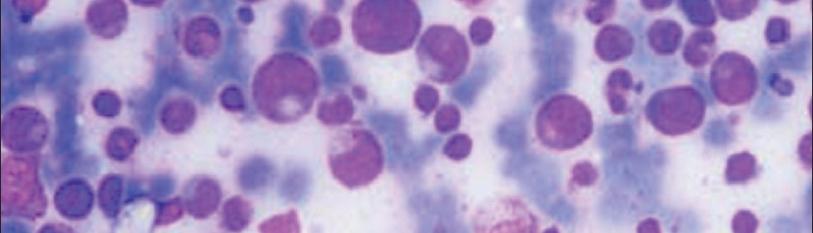
Pure red cell aplasia (PRCA)can be inherited (Diamond Blackfan Anaemia (DBA) or acquired (aPRCA), This PRCA gets further sub classified as: B19 Parvovirus - associated (transient) aplastic crises (TAC) [1]; drug associated cases [2] (like alluopurinol, azathioprine, diphenylhydantoin, rifampicin, valproic acid, etc.); primary idiopathica PRCA with different (immune) etiologiesas well as; secondary aPRCA correlated with other conditions like a) B cell dyscrasi as (chronic lymphocytic leukaemia [CLL] [3]. Waldenstrom macro globuloinemia [4], monoclonal gammopathy of undetermined significance (MGUS) [5] as well as multiple myeloma [6], T cell lympho proliferative disorders (large granular lymphocytic (LGL) [7,8], or solid organ malignancies (usually thymoma) [9] and b) collagen vascular/autoimmune process with a PRCA overlap [10-13]. Myelodysplastic syndromes (MDS) can mimic PRCA morphologically [14]; aPRCA might also be a precursor of acquired aplastic anaemia (AA). Adult acquired pure red cell aplasia (aPRCA) is a rare syndrome that is characterized by a severe normocytic anaemia, reticulocytopenia, the absence of erythroblasts from an otherwise normal bone marrow [15]. Secondary PRCA is usually dominated by the underlying disease. B19 Parvovirus-associated is secondary to the lytic activity of the virus on pronormoblasts [16] that is seen as large proerythroblasts with vacuolated cytoplasm as well aspseudopodia (giant pronormoblasts). Following ruling out of viral causes, congenital disease as well as drug reactionidiopathic PRCA would be the commonest cause, with the majority of cases believed to be by auto reactive T cells. This is mainly through selective T or NK cell mediated killing of erythroid colony (CFU-E) and burst (BFU-E) forming units, thus inhibiting red cell precursor progression to mature erythrocytes (Figure1) [7,17].
Figure 1: Courtesy reference no-20-Pathogenesis of pure red cell aplasia (PRCA) in our cohort. (A) Different causes of PRCA affect red cell production in different ways. Parvovirus causes direct cytolysis of erythroid precursor cells. Several drugs are implicated in causing PRCA, probably through a direct toxic effect. EPO antibodies can recognize antigens at the erythroid burst forming unit (BFU-E) level and cause PRCA. There is a wide range of antigen recognition by CTL exhibiting a polyclonal response, seen as negative TCR (T-cell gene rearrangement) by testing, which, however, still causes PRCA, probably by direct cytotoxicity. At the other end of the spectrum are LGLs that are monoclonal with STAT3 mutations and can recognize antigens at the erythroid precursor level, and thus cause PRCA. (B) Flow cytometry Vβ analysis of the peripheral blood of individual representative patients from the cohort shows clonal skewing. Illustration shows a spectrum of polyclonal to oligoclonal to monoclonal response of CTL in individual patients with PRCA.
Similar to acquired neutropenia, idiopathic PRCA is classically T cell mediated .While auto immune PRCA is mediated by antibodies is
Case Report
A 30 year old patient married for 7 years presented on18/11/2019 with history of 1 full term normal delivery(FTND), six year back on with a live born (LB)/male (M) alive & well. Then 4 years back following an episode of high grade fever upto 104 degree F fell unconscious or following removal of breast lump somewhere at that time and although histopathological examination (HPE) not given sample was sent to Bombay but report not collected and now misplacedby the centre in Nakodar. Since, then her haemoglobin keeps dropping off and on. Receives Blood Transfusion (BTs), it comes up but soon it goes down within a week to a month. He has visited Dayanand Medical College, Christian Medical College, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh. Has received almost over 110 blood transfusions (BTs) till now. On examination weight 55kg, height 164cm with a BMI of 20.44kg/m,BP-110/76 mmHg. Cycles are regular 5/30 average flow. Went to PGIMER on 12/6 /17 where investigations done were parvo virus serology antinuclear antibody (ANA), CECT Chest, serum ferritin. Reports available antinuclear antibodies AB-IFA HEP2,Serum positive on 17/5/16 from Ranbaxy lab, Primary dilution 1:40, primary intensity (Method immunofluorescence microscopy), antinuclear antibodies (ANA) Pattern ((Method immunofluorescence microscopy), speckled on AF -1+, Serum ferritin 1221 ng/ml (10-200) and 1179 in 2 occasions. She was put on cyclosporine 100mg morning and 150 mg hs, ii) tab desferox 1gm od, iii) tab wysolone 50 mg od following breakfast, tab pantocid 40mg od, tab shelcal 1 bd, vitamin D3 sachet daily for 7 days she was a febrile, no splenomegaly was found on examination. On 11/5/17-Bone Marrow (BM) Examination was done on the day of BM CBC- Hb-4.2 g, PCV-12.2.RBC density-1.51(4.0-5.2), MCV-80(80-100, MCH27. 45(26-34)pg, MCHC-g/dl 34.12(31-37) Red cell distribution width RDW-CV%-17(11.6-14.5) Reticulocyte Count -%=0.1%(1.0-2.7) retic 0.17, platelet -380(150-450, TLC -5100(4-11), DLC -P51 L39, M7 E1ESR-80-.5. Clinical Impression (CI), Reduced RBC density, Mild anisopoikilocytosis. Normocytichypochromic red blood cells, HIV, HCV, HBs Ag-Non reactive, HIV antibody-negative, HCV antibody-negative.
Bone marrow examination-findings
- Blasts-i, Promyelocyte-1 Myelocyte -24 Meta Myelocyte-08
- Polymorphs-40 Lymphocytes-22 Eosinophils-02
- NE:E Ratio M:E Ratio 37.5:1
- Clinical Impression (CI)-Erythropoiesis reduced-only early intermediate precursors, no viral cytopathic effects (giant proerythroblasts, inclusions) etc. is seen thrombopoies is is adequate.
- Erythroid precursors -02%-no significant dyshaemopoies is in any of lineages. Perl’s stain smear is particular macrophage iron.
Trephine Biopsy
Bilateral-2cm each shows hypercellular marrow spaces (overall cellularity 80-90%) with marrow done. Marked granulocytic and megakaryocytic hyperplasia along with mild interstitial increase in lymphocytes, focally also plasma cells and occasional lymphoid aggregate formation. Erythroid cells are markedly reduced. Reticulin fibrosis present diffusely. Interpretation-Hypercellular Bone Marrow shows marked erythropenia, prominent Lymphocytes and low grade fibrosis. Findings are suggestive of an autoimmune disease. Adv-collect limited panel flow cytometry report. Repeated LFT /RFT/Thyroid function test was normal. 22/1/18CT Chest-no intra thoracic mass/collection seen, mild glandular tissue thickening seen on right side of breast, no calcification seen.Likely inflammatory, lungs normal, no consolidation, no pleural/pericardial effusion. Asymmetric hepatomegaly-left lobe predominantly enlarged and few small hypodense areas in both lobes liver? partial filling of vein. Now was referred for a mass in ovaries trans vaginal sonography (TVS) revealed a solid mass in left ovarymeasuring 50x35.8 mm and right ovary vague mass multiseptate 33x30.5 mm with fluid in pouch of douglas. Only latest LFT increased SGOT/PT was observed.
Patient was asked to retrieve histopathology examination (HPE) report of breast lump biopsy and plan paracentesis is but unfortunately HPE report was misplaced as 4 yrs old but by that time TVS revealed fluid in pouch of douglas had resorped and left ovarian cyst had disappeared and in left ovary endometrioma was seen hence she was put on desferoxamine (in view of continuing packed cell transfusions and high ferritin earlier twice) as well as steroids, that were restarted and in view of low levels of Hb further from 4 to 2 Packed Cell transfusion given and mifegest was started-after 2wksdanazol 200mg bd was added on14/12/2019. Since then she has received mifigest for 4mths anddanazol for 41/2 months but due to shortage of desferoxamine she could not maintain desferoxaxamine in take. Further since haemoglobin maintaining around 4 gm addition of metoclopramide was also done about a month back 10mg od but still her need for blood has not finished although she has started feeling better generally and needs packed red cell transfusion monthly now with lesser frequency and is able to carry out daily chores. On 12/3/2020 Latest CBC reports are Hb-4.4gm TLC6900, DLC-p53L44,M1, E3 RBC Count 1, 47 (4.5 -6.5 million/cumm) Platelets-2.5 lacs (1.5-4.5).
Discussion
Ours is one of the rare cases of a PRCA having 2 known autoimmune diseases like SLE along with endometriosis who failed to respond to 8 months of cyclosporine 100/150mg in a day as well as corticosteroids like prednisolone 50mg in 2017 after which she developed side effects with cyclosporine A and she just stopped going to the tertiary institute PGIMER. We used the same definitions for complete remission (CR )as used by Balasubramaniam et al. [20] like rise in reticulocyte count, along with Hb, as well as becoming transfusion independent followed by subsequent normalization of Hb levels following 8wks of initiating the treatment ,while partial remission (PR) was defined when there was no appropriate increase in reticulocyte count as well as patient was still anaemic, but her transfusion need became less frequent than it was before starting the therapy .No response (NR) was defined when none of above criteria were met by the end of 8 wks. Our pt received therapy for 8 months following which she abandoned therapy in view of? No CR or PR and developing? liver or renal side effects and did not get any proper treatment for 2 years when she again came to us with a suspicion of a malignant ovarian tumour in both ovaries with fluid in pouch of douglas (POD)-in view of her low haemoglobin and severe generalized weakness we could not take fluid from pouch of douglas as could not give her GA with low Hb and luckily in mean time lots of fluid resorbed from POD and appearance of left ovary was suggestive of endometrioma and with the idea of stopping more blood loss we put her on mifepristone 50mg alternate dayto achieve amenorrhea and then further reading about earlier reports of remissions with danazol from both angles that is for remission of aPRCA as well asendometrios is control, along with corticosteroid upto 50mg in view of her being intolerant to cyclosporine. A following roughly 4 months of danazol and mifepristone when we were forced to omit mifepristone and patient having lost her husband due to cirrhosis development secondary to HCV positive now she is in a bad financial crises and it is difficult for her to procure desferoxamine and arrange more packed cell transfusions so we added, metoclopramide 10mg as well. Remissions have been achieved by immunosuppressive treatment with corticosteroids(CS), cyclophosphamide, cyclosporine A (CsA), antithymocyte globulin (ATG), antiCD20 monoclonal antibody rituximab, as well as the anti CD-52 monoclonal antibody alemtuzumab [reviewed in ref no- 21]. Means [22] documented that Cs A had better actions on PRCA as compared to CS based on literature review. But a Japanese nationwide survey pointed that CsA as well as CS gave similar remissions in primary PRCA. Thus Wu et al, analysed73 patients in 2 institutions. Induction therapy had Cs A(n=21), CS(0.5-1mg/kg/d(n=21), or CsA (5mk/kg/d) with CS combined (n=31), remission was achieved in 16/21(76.2%), 10/21(47.6%) and 21/31(71.0%) patients respectively. Minimum period needed for evaluation was defined as 4 weeks (range1-6mths). Higher Clinical Remission (CR) rate was got in CsA with CS combined therapy and primary PRCA were the influence factors for CR rate. Twenty seven percent patients relapsed due to discontinuation or tapering therapy and 19 of patients regained response by increasing the dose of original regimens or changing to other immunosuppressive therapy .CR to induction therapy was a correlative factor for death (p=0.035). In secondary PRCA, 9/26 achieved CR (34.6%, 3 LGL and 6 thymoma) and 6 patients [21]. As our patient developed liver function problems? Renal problems with cyclosporine she left both cyclosporine and corticosteroids for 2 years with no proper therapy other than intermittent blood transfusions .In view of reading that danazol had efficacy in DBA we started danazol 200mg bd besides starting mifepristone (a Selective Progesterone Receptor Modulator [SPRM]) with the diagnosis of endometrioma in left ovary so that amenorrhea could be achieved and blood loss during cycles avoided [23]. Further Shao et al. used danazol in an aPRCA patient refractory to cyclosporine and corticosteroids where ankylosing spondyl it is was present along with blood transfusions with desferioxamine like in our case, and then rHuEPO (40,000iu/w via subcutaneous injection and following 18mths patients reticulocyte count as well as Hb improved and they gradually tapered the prednisone to 7.5mg/d [24]. Similarly Chan et al, reported successful therapy of aPRCA in a patient of SLE [25]. In our patient we gave 2 doses of erythropoiet in 400iu although it was not recombinant, besides iv albumin infusions. Further since in DBAit has been reported that metoclopramide alone was effective [26], we added metoclopramide as well, and we plan to add leucine that was also effective in DBA [27]. We will observe the patient upto 18 months that is the time taken by other patients who received danazol and try giving cheaper nandrolone [28] as well with some reports of anabolicsteroids helping in view of poverty although she is already getting danazol another anabolic steroid and patient not affording repeated ferritin tests along with blood transfusions .Mostly idiopathic aPRCA responds to calcineurin inhibitors (cyclosporine A) with a tapering steroid that gives overall response rate of 76% as most respond to T cell immunosuppression. Although we could have started cyclophosphamide with corticosteroids we preferred to use danazol in view of doubt of malignancy and side effect of cyclophosphamide is stimulating malignancy and prevention of bacterial and viral infections.
Figure 2: Courtesy reference no-20-Treatment algorithm for immune-mediated PRCA in our patient cohort. Cyclosporine or cyclophosphamide with a steroid taper is the first-line choice of treatment in both idiopathic and LGL- related PRCA. Maintenance treatment with immunosuppressive therapy is usually needed, and varies based on the sustainability of the response obtained (see text for details). Methotrexate is used in a salvage setting in LGL/PRCA, but has no role in idiopathic PRCA. Alemtuzumab is one of the commonly used salvage options in refractory PRCA.
With 4 months of this therapy she has developed PR. We will hope she recovers with this therapy over 18mths otherwise will have to move to alemtuzumab (Campath) or intravenous immunoglobulins as in our case we had ruled out parvovirus infection and IVIG is more effective in parvovirus or hypogamma globulinemia or rituximab (that is more efficacious in B cell problem like myasthenia gravis) as per Balasubramaniam et al, [20] flow diagram, ATG, anabolic steroids, tacrolimus or Bartlozomib, tacrolimus, ATG, abatacept, ustenikumab or other RA drugs if RA+ (Figure 2).
References
- Brown K, Young N. (1995) Parvovirus B19 infection and haematopoiesis. Blood Rev. 9(3):176-82.
- Thompson DF, Gales MA. (1996) Drug induced pure red cell aplasia. Pharmacotherapy. 16(6):1002-8.
- Stohlman F, Quesenbury P, Howard D, Muller M, Schur P. (1971) Erythroid aplasia: an autoimmune complication of chronic lymphocytic leukaemia. Clin Res.19:566.
- Masauzi N, Tanaka J, Watanabe M, Matuura J, Morii K, et al. (1993) Primary Waldenström's macroglobulinemia associated with pure red cell aplasia in which Ts/c lymphocytes inhibiting erythroid precursors were detected. Jpn J Clin Hematol 34(3):355-61.
- Kobayashi T, Hanada T, Sato Y, Shibuya A, Ninomiya H, et al. (1987) A case of pure red cell aplasia. With monoclonal gammopathy: immune-mediated inhibition of erythropoiesis. Rinshoketsueki. 28(11):2029-033.
- Orchard J, Myint H, Hambin TJ. (1997) A patient with myeloma who still has pure red cell aplasia. Despite the most intensive immune modulation. Leuk Res. 21(4):353-54.
- Abkowitz JL, Kadin ME, Powell JS, Adamson JW. (1986) Pure red cell aplasia: lymphocyte inhibition of erythropoiesis.Br J Haematol. 63(1):59-67.
- Levitt LJ1, Reyes GR, Moonka DK, Bensch K, Miller RA, etal.(1988) Human T cell leukemia virus-I-associated T-suppressor cell inhibition of erythropoiesis in a patient with pure red cell aplasia and chronic T gamma-lympho proliferative disease. J Clin Invest. 81(2):538-48.
- Bailey RO, Dunn HG, Rubin AM, Rittacio AL. (1988) Myasthenia gravis with thymoma and pure red cell aplasia. Am J Clin Pathol. 89(5):687-93.
- Casadevall N, Dupuy E, Molho-Sabatier P, Tobelem G, Varet B, et al. (1996) Autoantibodies against erythropoietin in a patient with pure red cell aplasia.NEngl J Med. 334(10):630-33.
- Dessypris EN, Krantz SB, Roloff JS, Lukens JN. (1982) Mode of action of the Ig G inhibitor of erythropoiesis in transient erythroblastopenia of children. Blood. 59(1):114-28.
- Duchmann R, Schwating A, Poralla T, Zum Buschenfelde KHM, Hermann E. (1995) Thymoma and pure red cell aplasia in a patient with systemic lupus erythematosus. Scand J Rheumatol. 24(4):251-54.
- Peschle C, Marmont AM, Marone G, Genovese A, Sasso GF, et al. (1975) Pure red cell aplasia:studies on an Ig G serum inhibitor neutralizing erythropoietin. Br J Haematol. 30(4):411-17.
- Williamson P, Oscier D, Bell A, Hamblin T. (1991) Red Cell Aplasia in myelo dysplastic syndrome. J Clin Pathol. 44(5):431-32.
- Dessypris EN, Lipton JM, Greer JP, Forester J, Lukes JN, et al. (2004) Red Cell aplasia. Wintrobe’s Clinical Haematology 11thed Philadelphia, PA: Lippincott Williams &Wilkins. 1421-7.
- Young N. (1988) Haematologic and haematopoietic consequences of n B19 Parvovirus infection. Semin Haematol. 25(2):159-72.
- Hirayama Y, Nagai T, Ohta H, Koyama R, Matsunaga T, et al. (1997) A case of pure red cell aplasia accompanied with granular lymphocytic leukaemia the tumor cells of which suppressed colony formation of BFU-E, and which was successfully treated by cyclophosphamide and cyclosporine. Jpn J Clin Hematol. 38(11):1206-11.
- Casadevall N. (2002) Pure red cell aplasia and anti-erythropoietin antibodies in patients treated with epoetin. N Engl J Med. 346(7):469-75.
- Murray W, Webb J. (1966) Thymoma associated with hypogammaglobulinaemia and pure red cell aplasia. Am J Med. 41(6):974-80.
- Balasubramaniam SK, Sadaps M, Thota S, Aly M, Przychodzen BP, et al. (2018) Rational management approach to pure red cell aplasia. Haematologica. 103(2):221-30.
- Wu X, Yang Y, Lu X, Wang S, Wang S, Hong M, et al. (2019) Induced complete remission faster in adult patients with acquired pure red cell aplasia by combining cyclosporine A with corticosteroids. Medicine 98:41(e17425).
- Means RT Jr. (2016) Pure red cell aplasia. Blood 2016;128:2504-9
- Chai KY, Quijano CJ, Chiruka S. (2019) Danazol: an effective and underutilized treatment options in Diamond Blackfan Anaemia. Case Rep Hematol. 2019:4684156.
- Shao X, Wei W, Zhao Y, Liang X, Lu Q. (2019) Acquired pure red cell aplasia in a patient with ankylosing spondylitis –a case report and literature review. Medicine. 98:27(e16160).
- Chan AY, Li EK, Tam LS, Cheng G, Choi PC, et al. (2005) Successful treatment of pure red cell aplasia associated with systemic lupus erythematosus with oral danazol and steroid. Rheumatol Int. 25:388-90.
- Akiyama M, Yanagisawa T, Yuza Y, Yokoi K, Ariga M, et al. (2005) Successful treatment of Diamond Black fan Anaemia with metoclopramide. Am J Haematol. 78(4):295.
- Pospisilova D, Cmejlova J, Hak J, Adam T, Crneijla R. (2007) Successful treatment of a Diamond Blackfan Anaemia patient with amino acid leucine. Haematologica. 92(5):e66.
- De Marchi PN, Sueur Vieira ANL, Antunes Ribeiro JF, Geraldes SS, Rodriques Ramos PR, et al. (2017) Use of Nandrolone Decanoate in Treatment of Pure Red Cell Aplasia Secondary to Diclofenac Administration: A Case Report. Top Companion. Anim Med. 32(1):44-7.

