Fluid Creep in Critically ill Patients: Time to Sop the Flood
Ahmed N Ghanem*
NHS The UK and Mansoura University, Faculty of Medicine Egypt; Consultant Urologist Surgeon-Retired Independent Investigator & Scientist, Free Lance Author, Dreamer & White Revolutionary, Egypt
*Corresponding author: Ahmed N Ghanem, NHS The UK and Mansoura University, Faculty of Medicine Egypt; Consultant Urologist Surgeon-Retired Independent Investigator & Scientist, Free Lance Author, Dreamer & White Revolutionary, Egypt.
Citation: Ghanem AN. (2022) Fluid Creep in Critically ill Patients: Time to Sop the Flood. Genesis J Surg Med. 1(1):1-06.
Received: September 12, 2022 | Published: September 30, 2022
Copyright©️ 2022 Genesis Pub by Ghanem AN. This is an open-access article distributed under the terms of the Creative Commons Attribution4.0 International License (CC BY 4.0). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are properly credited.
DOI: https://doi.org/10.52793/GJSM.2022.1(1)-5
Abstract
Fluid Creep (FC) is a new name for an old phenomenon of fluid retention in hospitalized critically ill Patients after resuscitation for major trauma, shock, and sepsis. The phenomenon is typically observed in patients suffering from the acute respiratory distress syndrome (ARDS). It is associated with high morbidity and mortality among the critically ill patients with ARDS. It has been reported since fluid therapy became the mainstay for shook and trauma resuscitation Fluid creep is not really a new phenomenon, but the word creep may be relatively new use here. It has been consistently reported since the use of fluid therapy on a wide scale during World War 2. It was reported under the names of “fluid retention, fluid overload, positive fluid balance, fluid therapy complications and volumetric overload”. This phenomenon is both preventable and treatable.
Keywords
Fluid creep; Fluid overload; Fluid retention; Volumetric overload; Shock; Resuscitation
Introduction
This excellent article reviews the current knowledge and understanding of this phenomenon [1] which demonstrate that authors of the concerned authorities and physicians at large remain unaware of its true aetiology and best management. It also discusses Starling’s law as the main scientific foundation for fluid therapy in the shock resuscitation and acutely ill patients but falls short of incriminating it as the culprit for causing the phenomenon of fluid creep. My research that spans over the last 40 years and abundantly reported over the last decade has documented 13 new scientific discoveries in physics, physiology, and medicine [2] that form the new scientific foundation for fluid therapy in shock management [3].
My research has demonstrated that Starling’s law is wrong on both of its forces and is the reason why good physicians are being misled into giving too much fluids during shock management. The discovery of the hydrodynamics of the porous orifice tube akin to capillary provide the correct replacement for the wrong Starling’s law [4,5]. The tree branching law corrects 2 widely received misconceptions on the capillary circulation [6].
Volume overload (VO) or fluid overflow (FC) occurs during fluid resuscitation for shock treatment in critically ill patients. It is an iatrogenic condition. Most cases of VO or FC begin with flooding, where a large amount of fluid is injected in a short period of time. It is of two types: Type 1 is induced by sodium-free fluids and is characterized by acute severe dilutional hyponatraemia of <120 mmol/l for which the TUR syndrome is an example, and Type 2 is induced by sodium-based fluids and presents as ARDS. VO presents initially with a cardiovascular shock that is mistaken for one of the well-known shocks and gets wrongly treated with further volume expansion [7,8]. The magnitude of VO or FC is shown in figures 1 and 2. Table 1 shows that VO or FC is most significant factor in the patho-etiology of the TUR syndrome and ARDS. Table 2 summarizes the clinical picture of the conditions. Table 3 shows the biological patients’ data and changes of serum solutes and therapy outcome. The first report on ARDS documented VO or FC of 12-14 litres ic dead patients [9]. A recent huge, multi-center prospective study on ARDS document fluid retention or VO or FC of 7-10 liters in surviving ARDS patients [10].
Also, my discoveries have demonstrated that both types have an effective lifesaving therapy using hypertonic sodium therapy (HST) of 5% NaCl and 8.4% NaCo3 [11]. This HST should be given instantly, rapidly, and adequately as early as possible in the course of the illness immediately after suspecting the diagnosis. By the end of this HST that lasts one hour giving less than one liter, the patient sheds urine of 4.5-5 Liters of the fluid that was retained in his body. This massive urinary output should not be replaced by further fluid creep. The response to HST on correcting serum osmolality and sodium with matching remarkable clinical improvement is shown in figure 3 [Figure1-4].
Review and Conclusion
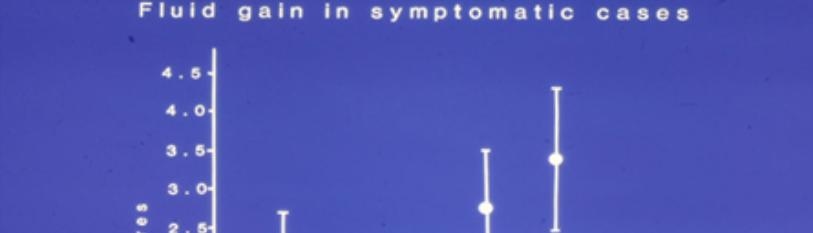
Figure 1 shows the means and standard deviations of volumetric overload in 10 symptomatic patients presenting with shock and hyponatraemia among 100 consecutive patients during a prospective study on transurethral resection of the prostate. The fluids were of Glycine absorbed (Gly abs), intravenously infused 5% Dextrose (IVI Dext) Total IVI fluids, Total Sodium-free fluid gained (Na Free Gain) and total fluid gain in litres. This fluid gain occurred during the time of surgery which is less than one hour.
Figure 1: Shows the means and standard deviations of volumetric overload in 10 symptomatic patients presenting with shock and hyponatraemia among 100 consecutive patients during a prospective study on transurethral resection of the prostate.
Figure 2 shows volumetric overload (VO) quantity (in litres and as percent of body weight) and types of fluids. Group 1 was the 3 patients who died in the case series as they were misdiagnosed as one of the previously known shocks and treated with further volume expansion. Group 2 consisted of a series of 10 patients who were correctly diagnosed with volume-overload shock and treated with hypertonic sodium therapy (HST). Group 3 were 10 patients who were seen in the prospective study and subdivided into 2 groups; Group 3.1 of 5 patients treated with HST and Group 3.2 of 5 patients who were treated with guarded volume expansion. All this VO or FC occurred during less than one hour.
Figure 2: Shows volumetric overload (VO) quantity (in litres and as percent of body weight) and types of fluids.
Figure 3: Shows mean changes in measured serum osmolality (OsmM) and calculated osmolality (OsmC) in patients with the TUR syndrome.
Figure 3 shows mean changes in measured serum osmolality (OsmM) and calculated osmolality (OsmC) in patients with the TUR syndrome comparing those infused with 5% hypertonic sodium (solid lines) and those treated conservatively (slashed lines). OsmC was calculated from the formula 2xNa+urea+glucose in mmol/l of serum concentration thus reflecting changes in serum sodium concentration. The vertical dotted line represents the start of operation (Time B) followed by C, C1, C2 (end of one hour treatment) and D (next morning), respectively.
Table 1 shows the multiple regression analysis of total per-operative fluid gain, drop in measured serum osmolality (OsmM), sodium, albumin, Hb and increase in serum glycine occurring immediately post-operatively in relation to signs of the TURP syndrome. Volumetric gain and hypo-osmolality are the only significant factors.
|
P |
T Value |
Std. Value |
Std. Err |
Value |
Parameter |
|
- |
- |
0.773 |
- |
- |
Intercept |
|
0.0007 |
3.721 |
1.044 |
0.228 |
0.847 |
Fluid Gain (l) |
|
0.0212 |
2.42 |
-0.375 |
00.014 |
0.033 |
Osmolality |
|
0.0597 |
1.95 |
0.616 |
0.049 |
0.095 |
Na+ (C_B) |
|
0.4809 |
0.713 |
0.239 |
0.087 |
0.062 |
Alb (C_B) |
|
0.2587 |
1.149 |
-0.368 |
0.246 |
-0.282 |
Hb (C_B) |
|
0.4112 |
0.832 |
-0.242 |
5.975E-5 |
-4.973E-5 |
Glycine (C_B) |
Table 1: Shows the multiple regression analysis of total per-operative fluid gain, drop in measured serum osmolality (OsmM), sodium, albumin, Hb and increase in serum glycine.
Table 2 shows the manifestations of VOS 1 of the TURP syndrome for comparison with ARDS manifestations induced by VOS2. The manifestations are the same but one vital organ-system may predominate.
|
Cerebral |
Cardiovascular |
Respiratory |
Renal |
Hepatic & GIT |
|
Numbness |
Hypotension |
Cyanosis |
Oliguria |
Dysfunction |
|
Tingling |
Bradycardia |
FAM4 |
Annuria8 |
Bilirubin ↑ |
|
SBB1 |
Dysrhythmia |
APO)5 |
Renal failure or |
SGOT ↑ |
|
COC2 |
CV Shock* |
RA6 |
AKI9 |
Alkaline Phosph |
|
Convulsions |
Cardiac Arrest |
Arrest |
Urea ↑ |
GIT symptoms |
|
Coma |
Sudden Death |
CPA7 |
Creatinine ↑ |
DGR10 |
|
PMBCI 3 |
- |
Shock lung |
- |
Paralytic ileus |
|
- |
- |
ARDS$ |
- |
Nausea & Vomiting |
Table 2: Shows the manifestations of VOS 1 of the TURP syndrome for comparison with ARDS manifestations induced by VOS2.
Table 3 shows the mean summary of data on biochemical abnormalities, therapy and outcome comparing the 3 groups of 23 case series patients whose VO is shown in (Figure 2). Group 1 was the 3 patients with ARDS and fluid creep. who died and had post-mortem examination, Group-2 were a series of severe TURP syndrome cases successfully treated with hypertonic sodium therapy (HST), and Group-3 were 10 patients encountered in this prospective study was randomized between conservative treatment (CT) (3.2) and HST (3.1). The significant changes of serum solute contents are shown in bald font with the corresponding p- value. Most of the patients showed manifestation of ARDS of which the cerebral manifestation predominated, being on initial presentation (Regional Anaesthesia) and representation of VOS 1 (General Anaesthesia). However, most patients were provided with large volume of saline that increased the serum sodium to near normal and the clinical picture turned to be worse. They suffered VOS2 that caused ARDS.
|
1 |
Gr1 |
Gr2 |
Gr3 |
Gr3.1 |
Gr3.2 |
Normal |
Units |
|
|
2 |
Number of patients 3 |
10 |
10 |
5 |
5 |
mean |
- |
|
|
3 |
Age 71 |
70 |
75 |
72 |
78 |
72 Years |
- |
|
|
4 |
Body weight (BW) 69 |
70 |
68 |
71 |
65 |
69 Kg |
- |
|
|
5 |
Postoperative serum solute concentration |
- |
Preoperative |
|||||
|
6 |
Osmolality |
271 |
234 |
276 |
282 |
271 |
292 |
Mosm/1 |
|
7 |
Na+ |
110 |
108 |
120 |
119 |
121 |
139 |
Mmol/1 |
|
8 |
Ca++ |
1.69 |
1.79 |
1.85 |
1.84 |
1.86 |
2.22 |
'' |
|
9 |
K+ (P<.05) |
5.6 |
4.8 |
5 |
4.9 |
5 |
4.46 |
'' |
|
10 |
Co2 (P=.002) |
23 |
23 |
25.5 |
24 |
26.4 |
27.3 |
'' |
|
11 |
Glucose |
13.2 |
17.3 |
16.4 |
15.9 |
16.9 |
6.2 |
'' |
|
12 |
Urea (P=.0726) |
26.5 |
9 |
6.6 |
6.8 |
6.4 |
6.7 |
'' |
|
13 |
Bilirubin (P<.05) |
19 |
16 |
8 |
6 |
9 |
7 |
'' |
|
14 |
AST |
124 |
32 |
20 |
18 |
21 |
20 |
'' |
|
15 |
Protein |
43 |
52 |
48 |
44 |
52 |
62 |
g/l |
|
16 |
Albumin |
23 |
30 |
30 |
28 |
32 |
39 |
'' |
|
17 |
Hb (P=.0018) |
119.3 |
127.9 |
114.5 |
105.2 |
123.8 |
123.8 |
'' |
|
18 |
WCC (P<.005) |
18.9 |
16.2 |
7.5 |
7.8 |
7.2 |
8 |
per HPF |
|
19 |
Glycine |
- |
- |
10499 |
- |
- |
293 |
µmol/1 |
|
20 |
Therapy |
CT |
HST |
Randomized |
HST |
CT© |
- |
- |
|
21 |
Outcome |
Death |
Full Recovery |
- |
Full Recovery |
Morbidity |
- |
- |

