Endodontic Management of Developmental Anomalies Related to Shape of the Teeth: A Review
Aathees AS*
Post graduate student, Department of Conservative and Endodontics, Rajarajeswari Dental College, Bangalore
*Corresponding author: Aathees AS, Post graduate student, Department of Conservative and Endodontics, Rajarajeswari Dental College, Bangalore
Citation: Aathees AS. Endodontic Management of Developmental Anomalies Related to Shape of the Teeth: A Review. J Oral Med and Dent Res. 5(2):1-10.
Received: September 6, 2024 | Published: September 10 , 2024
Copyright© 2024 Genesis Pub by Aathees AS. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are properly credited.
DOI: https://doi.org/10.52793/JOMDR.2024.5(4)-73
Abstract
This article is a review on the various developmental anomalies related to shape of the teeth, and their management strategies under the endodontic speciality. These dental anomalies are congenital malformations that occur in a single tooth and can also be related to various syndromes. Hence it is of importance to know about the developmental anomalies. This article aims to illustrate the insights of developmental anomalies related to shape of the tooth, along with their management in endodontic view. Various treatment options for each anomalies are discussed based on the data available in the literature.
Keywords
Dental anomalies; Fusion and Gemination; Talons cusp; Dens invaginatus; Dilaceration
Introduction
Dental abnormalities create notable aesthetic and functional challenges within the teeth. Therefore, it is essential to carefully examine the factors contributing to their development [1]. Certain genetic factors have been identified as contributing to the emergence of different dental anomalies. Additionally, disruptions during tooth development can lead to variations in tooth number (agenesis/supernumerary teeth), size, shape, and position of tooth buds, impacting both permanent and primary dentition in both upper and lower jaws.
The maxilla and mandible, which support the upper and lower teeth respectively, form the essential hard tissue framework of the masticatory system. Despite serving a common function and containing a similar number of teeth, the development of the maxilla and mandible differ. This divergence contributes to the varied incidence of dental anomalies observed in each jaw [1].
Classification of developmental disturbances of teeth
Genetic tooth anomalies can be categorized in three main ways. First, it is essential to identify the type of anomaly, whether it involves number, shape, or both [2].
- Developmental disturbances in size of teeth
- Developmental disturbances in shape of teeth
- Developmental disturbances in number of teeth
- Developmental disturbances in structure of teeth
|
Category |
Name |
|
Number |
Missing teeth [2] Supernumerary teeth [2] |
|
Size and shape |
Peg shaped teeth Fusion [2] Gemination [2] Talons cusp [2] Dilaceration [2] Concrescence [2] Dens Invaginatus [2] Dens evaginatus / Enamel pearl [2] Taurodontism [2] |
|
Structure |
Amelogénesis imperfect [2] Enamel hypoplasia [2] Dentinogenesis imperfect [2] Dentin dysplasia [2] Regional Odontodysplasia [2] |
Developmental Anomalies in Shape of Teeth: Description
Gemination
Tannenbaum and Alling (1963) defined gemination as the formation of what appears to be two teeth from the same dental follicle, where there is evidence of an effort for the teeth to develop as distinct entities. [3]
Gemination, also known as double teeth, double formations, joined teeth, fused teeth, or dental twinning, is commonly observed in the anterior region of the maxilla [3].
Geminated teeth originate from an attempt to split a single tooth germ through invagination, resulting in a single tooth with two fully separate crowns; or a large crown that is incompletely divided with a single root and root canal, which can be confirmed through radiographic imaging.
The anomalous tooth has a larger mesial-distal diameter than normal and is counted as one. However the total number of teeth in the dental arch is otherwise normal [3].
The cause of geminated teeth is still not fully understood. Spouge proposed in 1973 that the condition may arise from trauma to the developing tooth bud. Several case studies indicate a hereditary predisposition for this anomaly. The mode of inheritance is likely either autosomal recessive or dominant with low penetrance. It is evident that gemination results from intricate interactions involving a range of genetic and environmental factors [4].
Fusion
A fused tooth is characterised by the joining of two teeth into a single enlarged structure, leading to a reduced tooth count when the anomalous tooth is considered as one. However, if the fused tooth involves a supernumerary tooth, the overall tooth count remains normal. This condition is also referred to as synodontism [4].
The cause of tooth fusion remains unclear, but one suggested factor is the influence of pressure or physical forces that bring two developing teeth into close contact. Genetic predisposition and racial variations have also been identified as contributing factors. This process involves interactions between the epithelial and mesenchymal germ layers, leading to irregular tooth morphology and increased size [4].
Fusion can occur in two forms: complete (total/true fusion) or incomplete (partial/late fusion), depending on the developmental stage at which it starts. When fusion begins before the calcification stage, the teeth fully unite, and the crown incorporates enamel, dentin, cementum, and pulp from both teeth. Incomplete fusion can happen at a later stage, resulting in a tooth that may have separate crowns but a shared root, with fused or separate pulp canals [3].
Fusion can lead to aesthetic issues and disruptions in occlusion due to crowding and irregular tooth shape. Deep grooves resulting from fusion can increase the risk of cavities and may lead to early pulp exposure [3].
Concrescence
Concrescence is a rare developmental anomaly where two fully formed teeth are joined at their root surfaces by cementum [4].
The exact cause of concrescence remains unclear, but many experts believe it may result from space restrictions during development, local trauma, excessive occlusal force, or local infection occurring after development [3].
Concrescence is commonly observed in the posterior maxillary region. It often involves a second molar whose roots are in close proximity to an adjacent impacted third molar. There have also been cases where there is concrescence of a third molar with a supernumerary tooth [3].
Dilaceration
The term "dilaceration," first used by Tomes in 1848, refers to a deviation or bend in the linear alignment between a tooth's crown and its root [4]. The term "dilaceration" is applied to teeth which have the long axis of either the whole or part of the root formed at an angle to the crown [3].
These deformities in permanent teeth can result from trauma to the primary tooth during the development of its permanent successor, causing a shift in the position of the calcified portion. Consequently, the remainder of the tooth forms at an angle [4].
Various other contributing factors have also been reported such as scar formation, developmental anomaly of the primary tooth germ, facial clefting, advanced root canal infections, ectopic development of the tooth germ and lack of space, effect of anatomic structures (Eg. cortical bone of the maxillary sinus, mandibular canal, or nasal fossa, which might deflect the epithelial diaphragm), presence of an adjacent cyst, tumour, or odontogenic hamartoma, mechanical interference with eruption (Eg. from an ankylosed primary tooth that does not resorb), tooth transplantation, extraction of primary teeth, and hereditary factors [3].
Dens Invaginatus
Dens invaginatus (DI), also known as the pregnant woman anomaly, extensive compound odontoma, or dens in dente, occurs due to an invagination on the external surface of the tooth crown before calcification. This invagination can vary from a shallow pit limited to the crown to a deep indentation extending into the root, sometimes reaching or surpassing the root apex [3].
The majority of cases are found in the maxilla, with maxillary lateral incisors being the most commonly affected, followed by central incisors, premolars, canines, and molars. The characteristic radiographic appearance of coronal DI is a pear-shaped invagination of enamel and dentin, with a narrow constriction at the opening on the tooth surface. The infolding enamel lining appears more radiopaque than the surrounding tooth structure, making it easier to identify [3]. Oehlers et al grouped coronal DI into three types according to the radiographic appearance [5]:
- Type I: An enamel-lined minor form occurring within the confines of the crown not extending beyond the cemento-enamel junction;
- Type II: An enamel-lined form which invades the root but remains confined as a blind sac. It may or may not communicate with the dental pulp;
- Type III A: A form which penetrates through the root and communicates laterally with the periodontal ligament space through a pseudo-foramen. There is usually no communication with the pulp, which lies compressed within the root;
- TYPE III B: A form which penetrates through the root and perforating at the apical area through a pseudo-foramen. The invagination may be completely lined by enamel, but frequently cementum will be found lining the invagination.
Infection, trauma, or pressure from the developing dental arch could cause dens invaginatus. Additionally, a localized growth failure or proliferation of part of the inner enamel epithelium might contribute to the invagination. Ohlers proposed that a distortion of the enamel organ and the subsequent protrusion of part of the enamel organ leads to the formation of an enamel-lined channel [3].
Dens Evaginatus
Dens evaginatus (DE) is a developmental anomaly of a tooth characterised by the formation of an accessory cusp. This cusp has been described as an abnormal tubercle, elevation, protuberance, excrescence, extrusion, or bulge. Other terms for this condition include tuberculated cusp, accessory tubercle, occlusal tuberculated premolar, Leong's premolar, evaginatus odontoma, and occlusal pearl. The term "dens evaginatus" is now preferred terminology and was first recommended by Oehlers in 1967 [5]. This rare anomaly involves the projection of an accessory structure above the adjacent tooth surface, characterised by enamel covering a dentinal core that typically includes pulp tissue. Occasionally, slender pulp horns extend to various depths within the dentinal core. The tubercles of dens evaginatus are distinct from the Carabelli cusp, a normal anatomical feature, as they contain a pulp core, unlike the Carabelli cusp, which lacks this structure [3].
When dens evaginatus appears in the anterior region, it is usually observed on the lingual surface and is described as a Talon's cusp [6]. It is commonly observed in maxillary lateral incisors and has been linked with syndromes such as Rubinstein-Taybi, Berardinelli-Seip, Mohr, Ellis-van Creveld, Sturge-Weber, and incontinentia pigmenti achromians syndrome. This anomaly varies in size, shape, length, and how it attaches to the crown, ranging from an enlarged cingulum to a large, well-defined cusp that extends beyond the tooth's incisal edge. The cusp consists of normal enamel and dentin containing varying extensions of pulp tissue. It may also connect with the incisal edge, resulting in a T-shaped or, if positioned lower, a Y-shaped crown contour [3].
Taurodontism
This dental anomaly lacks the typical constriction at the level of the cementoenamel junction (CEJ) and is characterised by elongated pulp chambers and an apical displacement of root bifurcation or trifurcation, resulting in a rectangular or "bull" shape [4].
This condition is often attributed to the failure of early invagination of the epithelial root sheath to form the root properly. Autosomal transmission of this trait has also been observed [4].
Witkop defined taurodontism as a condition where teeth exhibit large pulp chambers with apically displaced bifurcation or trifurcation, resulting in greater apico-occlusal height compared to normal teeth and lacking the usual constriction at the cementoenamel junction (CEJ). The distance from the root bifurcation or trifurcation to the CEJ is greater than the occluso-cervical distance. Taurodontism can occur in isolation affecting one or more teeth, or it may be associated with various syndromes such as Down syndrome, Klinefelter syndrome, etc. This condition can be unilateral or bilateral and is more commonly seen in permanent teeth than primary teeth. In 1928, Shaw classified taurodontism into hypo taurodontism, meso taurodontism, or hyper taurodontism based on the degree of apical displacement of the pulpal floor [4].
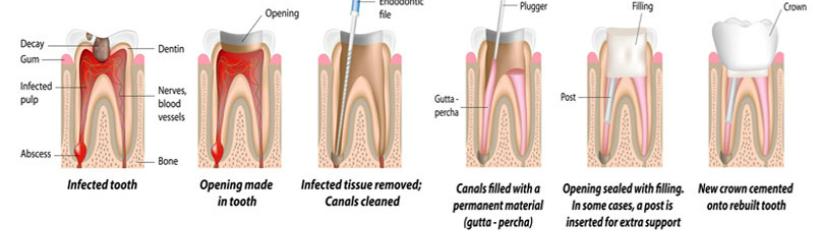
Endodontic management of various anomalies described above
Fusion and germination
Endodontic treatment of teeth with rare malformations demands extra attention during radiologic diagnosis and root canal procedures due to their unusual chamber and canal morphology. This atypical anatomy complicates accessing the pulp canal systems, determining the working length, and filling the large root canal. In such cases, using a three-dimensional CBCT scan before treatment is beneficial for accurately assessing the root and canal morphology [6].
The root canals of geminated and fused teeth can be cleaned and shaped to their full working lengths using rotary instruments [6].
During instrumentation, root canals should be irrigated with 2.5% sodium hypochlorite. After preparation, a final irrigation should be performed for one minute with 17% ethylenediaminetetraacetic acid (EDTA) and 2.5% sodium hypochlorite to remove the smear layer, followed by obturation [6].
IIn dental literature, various clinical approaches are recommended for managing fused or geminated teeth. These approaches include orthodontic treatment, tooth extraction, crown size reduction followed by restoration, sectioning of the fused teeth, or opting for no treatment at all [7].
Talon’s cusp (dens evaginatus)
According to Hattab et al., grinding the talon cusp is recommended when there is evidence of premature contact and occlusal interference. This procedure should be carried out gradually over consecutive visits spanning a 6–8-week period, allowing time for the deposition of reparative dentin and protecting the pulp [8]. Ozcelik and Atila suggested reducing the cusp in a single session, referring to this protocol as a "radical treatment" approach [9].
If the pulp is involved, both the reduction of the talon cusp and endodontic treatment should be considered for the affected tooth, depending on the degree of root development and pulp vitality, the endodontic treatment modality should be followed [10].
Dens Invaginatus
CBCT imaging can be highly effective for detecting dental anomalies like dens invaginatus (DI) and for planning root canal therapy and surgical treatments [11].
The thin layer of dentin and enamel between the pulp tissue and the invagination allows irritants to enter the root canal system, making the invagination a predisposing factor for caries. Additionally, pulp necrosis might occur in some cases due to incomplete enamel lining as a consequence of pulpal infection [12].
Treatment of dens invaginatus (DI) depends on the severity of the malformation and the stage at which it is diagnosed. Options range from simple prophylactic restoration or root canal treatment to surgical intervention. If detected at a very early stage, treatment may be limited to prophylactic restoration [13].
Root canal treatment (RCT) can focus specifically on the invagination, aiming to preserve pulp vitality [14,15] or removal of the DI followed by RCT [16]. The third option, in cases of DI that are difficult to access, is apicectomy of the involved tooth followed by RCT [17,18]. Extraction is considered the final resort for cases with complex anatomy or those that cannot be managed with endodontic treatment or periapical surgery [19].
In recent years, revascularization procedures have been introduced for treating necrotic teeth with open apices. However, due to the complex internal anatomy often seen in dens invaginatus (DI) cases, disinfecting the root canal system can be challenging. Proper disinfection of the root canal system is crucial for tissue regeneration, and therefore, the invaginated portion of a tooth with DI may not be suitable for regenerative endodontic procedures [20].
Dilaceration
Cleaning, shaping, and obturating curved root canals pose a challenge in endodontic treatment. The curvature of these canals must be carefully assessed and maintained throughout the procedure. The clinical approach varies depending on the severity of the root canal curvature [21]. While preparing the curved canals, the following principles should be closely followed [22].
- To preserve the original position of the apical foramen
- To achieve direct access to the curvature site in a straight line
- To avoid risks associated with curved canal anatomy, particularly the inner wall of the middle third and outer aspect of the apical third
- To use instruments that closely match the original canal shape while respecting its anatomy
The root canal should be sequentially filed with ample irrigation and recapitulation. Care must be taken to prevent ledge formation during preparation. Coronal flaring can be achieved using a Gates-Glidden (GG) drill. Nickel-titanium hand files are suitable for negotiating curved canals [23].
Non-cutting tip instruments made from nickel-titanium (NiTi) have demonstrated efficacy in maintaining root canal curvatures in numerous cases. However, dilacerated root canals are typically unsuitable for NiTi rotary instruments due to their severe and extensive curvature. All instruments used in highly curved canals should be discarded after use to prevent breakage within the canal, effectively treating them as single-use instruments [24].
Many dilacerated teeth, particularly anterior mandibular teeth, are often pulpless and infected with periapical inflammatory lesions. Therefore, the success of root canal treatment largely depends on thorough biomechanical debridement of the canals and effective elimination of microorganisms from the root canal system. In severely curved canals, copious irrigation, file recapitulation, and additional irrigation should be performed more frequently.
A multi-visit approach is recommended, incorporating interappointment intracanal medicaments to enhance treatment predictability. Intracanal medicaments play a crucial role in disinfecting the root canal system, particularly in areas that are difficult to access with mechanical instrumentation and irrigation. They also modify the intracanal environment to hinder microorganism survival. Given the well-documented benefits of calcium hydroxide in endodontic therapy, using this material as a medicament for dilacerated teeth is proposed. To facilitate delivery of calcium hydroxide to the apical third of dilacerated teeth, mixing it with glycerin instead of sterile water is suggested. Research indicates that glycerin is significantly more effective than water in achieving better length and density of filling in the apical third of curved canals [24].
The application of warm or thermoplasticized gutta-percha techniques may be more suitable in many cases, despite potential challenges posed by dilaceration. Studies indicate that in curved canals, the ThermaFil technique can yield comparable or superior apical sealing compared to the lateral condensation technique [24].
Taurodontism
Clinically, a taurodont tooth may appear normal, and therefore, its diagnosis should be made based on radiographs. Taurodont molars exhibit variations in the width of pulp chambers and canal structures, which can pose challenges during endodontic treatment [25].
Durr et al. suggested that the morphology of taurodont teeth can affect the position of the orifices, thereby complicating the shaping and filling of root canals [26]. Since the roots are short and the pulpal floor is placed apically, care must be taken to avoid any perforation of the pulpal floor [27].
Passive ultrasonic irrigation is a valuable adjunct for cleaning the root canal system because it can effectively remove more organic tissue, planktonic bacteria, and dentin debris compared to traditional syringe irrigation [28]. Henceforth, after shaping the root canal, cleaning should be completed with PUI or with a final flush of syringe irrigation [29-30].Tsesis et al. proposed using a combination of the lateral compaction technique and the warm vertical compaction technique for obturating a taurodont tooth [3].
Conclusion
A complete Case history, clinical examination, and radiographic examination can provide the information required for the diagnosis of such abnormalities. Teeth with these defects can be un-aesthetic due their irregular morphology, they also present high predisposition to caries, periodontal disease and spacing problems. As these abnormalities show variable anatomy of the root canal systems, endodontic treatment must proceed with utmost care and with use of appropriate and available advancements in the field of endodontics.
References
- Sella Tunis T, Sarne O, Hershkovitz I, Finkelstein T, Pavlidi AM, et al. (2021) Dental Anomalies' Characteristics. Diagnostics (Basel). 11(7):1161.
- Shafer, Hine, Levy. Shafers textbook of oral pathology. 8ed. Elsevier
- Shrestha A, MarlaV, Shrestha S, Maharjan IK (n.d.). Developmental anomalies affecting the morphology of teeth - a review.
- Thopte S, Khaire S, Nisa SU, Jadhav A. (2016) DEVELOPMENTAL ANOMALIES AFFECTING SHAPE OF TEETH. ResearchGate. 2(7):469-73
- Oehlers FA, Lee KW, Lee EC. (1967) Dens evaginatus, its structure and responses to external stimuli. Dent Pract. 17:239-44.
- Levitan ME, Himel VT. (2006) Dens evaginatus: literature review, pathophysiology, and comprehensive treatment regimen. J Endod 32:1-9.
- Ertaş ET, Atıcı MY , Arslan H, Yaşa B, Ertaş H, (2014) "Endodontic Treatment and Esthetic Management of a Geminated Central Incisor Bearing a Talon Cusp", Case Rep Dent, 123681.
- Alyahya A, Karkoutly K, Milly H,(2021) "Management of a Rare Case of Geminated and Fused Central Incisors in the Same Maxillary Dental Arch", Case Rep Dent, 5566827.
- Hattab F N, Yassin OM, Al-Nimri KS.(1996) Talon cusp in permanent dentition associated with other dental anomalies: review of literature and reports of seven cases. Journal of Dentistry for Children. 63(5):368–376.
- Ozcelik B, Atila B. Bilateral palatal talon cusps on permanent maxillary lateral incisors: a case report. European Journal of Dentistry. 5(1):113–16.
- Thirumalaisamy E, Baskaran P, Jeyanthi K, Kumar S. (2012) Talon cusp in fused teeth: a rare concomitant occurrence. Journal of Oral and Maxillofacial Pathology 16(3):411–13.
- Yalcin TY, Bektaş Kayhan K, Yilmaz A, Göksel S, Ozcan İ, et al. (2022) Helvacioglu Yigit D. Prevalence, classification and dental treatment requirements of dens invaginatus by cone-beam computed tomography. PeerJ. 10:e14450.
- (1997) Hulsmann M. (1997) Densinvaginatus:aetiology classification, diagnosis, and prevalence and treatment considerations. International Endodontic Journal. 30(2):79–90.
- Pallivathukal RG, Misra A, Nagraj SK, Donald PM.(2015) Dens invaginatus in a geminated maxillary lateral incisor. BMJ Case Rep. bcr2015209672.
- Jung M. (2004) Endodontic treatment of dens invaginatus type III with three root canals and open apical foramen. Int Endod J 37(3):205-13.
- Shadmehr E, Kiaani S, Mahdavian P. (2015) Nonsurgical endodontic treatment of a maxillary lateral incisor with dens invaginatus type II: a case report. Dent Res J (Isfahan) 12(2): 187–91.
- Schwartz SA, Schindler WG. (1996) Management of a maxillary canine with dens invaginatus and a vital pulp. J Endod. 22(9):493-6.
- Sauveur G, Roth F, Sobel M et al. (1997) Surgical treatment of a periradicular lesion on an invaginated maxillary lateral incisor (dens in dente). Int Endod J. 30(2):145-9.
- Fröner IC, Rocha LF, da Costa WF,Barros VM, Morello D, (1999) Complex treatment of dens invaginatus type III in maxillary lateral incisor. Endod Dent Traumatol 15(2):88-90.
- Hulsmann M. (1997) Dens invaginatus: etiology, classification, prevalence, diagnosis and treatment consideration. Int Endod J. 30(2):79-90.
- Shadmehr E, Farhad AR. Clinical management of dens invaginatus type 3: a case report. Iran Endod J. 6(3):129-32.
- Arora S, Gill GS, Setia P, Abdulla AM, Sivadas G, et al.(2018) Endodontic Management of a Severely Dilacerated Mandibular Third Molar: Case Report and Clinical Considerations. Case Rep Dent. 8:2018:7594147.
- Jafarzadeh H., Abbott P. (2007) Dilaceration: review of an endodontic challenge. Journal of Endodontics. 33(9):1025-30.
- Jain, Nidhi; Tushar, Suneja1.(2008) Curved canals: Ancestral files revisited. Indian Journal of Dental Research. 19(3):267-71.
- Jafarzadeh H., Abbott P. (2007) Dilaceration: review of an endodontic challenge. Journal of Endodontics. 33(9):1025-30.
- Simsek N, Keles A, Ocak MS. (2013) Endodontic treatment of hypertaurodontism with multiple bilateral taurodontism. J Conserv Dent.16(5): 477–79.
- Durr DP, Campos CA, Ayers CS. (1980) Clinical significance of taurodontism. J Am Dent Assoc. 100:378–81.
- Topcuoglu HS, KARATAŞ E, Arslan KE, Koseoglu MH, Evcil MS. (2011) The frequency of taurodontism in the Turkish population. J Clin Exp Dent. 3:e284–8.
- Tsesis I, Shifman A, Kaufman AY. Taurodontism: An endodontic challenge. Report of a case. J Endod. 2003;29:353–5
- Lee SJ, Wu MK, Wesselink PR.(2004) The effectiveness of syringe irrigation and ultrasonics to remove debris from simulated irregularities within prepared root canal walls. Int Endod J. 37(10):672-8.
- Passarinho-Neto JG, Marchesan MA, Ferreira RB, Silva RG, Silva-Sousa YT, et al. (2006) In vitro evaluation of endodontic debris removal as obtained by rotary instrumentation coupled with ultrasonic irrigation. Aust Endod J. 32:123–8.
- Maia RA, de Souza-Zaroni WC, Mei RS, (2015) Lamers F. Talon Cusp Type I: Restorative Management. Case Rep Dent. 2015:425979.
- Lee SJ, Wu MK, Wesselink PR.(2004) The effectiveness of syringe irrigation and ultrasonics to remove debris from simulated irregularities within prepared root canal walls. Int Endod J. 37(10):672-8.
- Passarinho-Neto JG, Marchesan MA, Ferreira RB, Silva RG, Silva-Sousa YT, et al. (2006) In vitro evaluation of endodontic debris removal as obtained by rotary instrumentation coupled with ultrasonic irrigation. Aust Endod J. 32:123–8.

