Dušan Petrović*
Center for Radiology and MRI, University Clinical Center of Serbia, Belgrade
*Corresponding author: Dušan Petrović, Center for Radiology and MRI, University Clinical Center of Serbia, Belgrade.
Citation: Dusan Petrovic. (2023) Autoimmune Encephalitis Clinical and Radiological (Mri) Correlation: Clinical Case Report. Genesis J Surg Med. 2(2):1-6.
Received: August 21, 2023 | Published: October 09, 2023
Copyright©2023 by Petrovic D. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
DOI: https://doi.org/10.52793/GJSM.2023.2(2)-16
Abstract
A 62-year-old man was admitted to the Emergency Department of the University Clinical Center of Serbia for transient and acute encephalitis syndrome. The patient`s symptoms included a dominant epileptic clinical presentation with the crisis of consciousness to the type of tonic- clinical convulsions and changed behavior (5 days before its clinical admission) in terms of weaker communication with occasional moments of aggressiveness. Brain computerized tomography (CT) was performed and showed only a hippo attenuated lesion posterocerebear left which answers first to arachnoid cist (differentially also possible chronicle ischemic lesion).
Keywords
Brain magnetic resonance imaging; Ischemic periventricular leukoencephalopathy; Brain computerized tomography
Introduction
Brain Magnetic Resonance Imaging (MRI) including diffusion-weighted MRI imaging was performed and showed: cortical reductive changes, ischemic periventricular leukoencephalopathy, microangiopathic changes, chronic ischemic change with marginal gliosis cerebral caudoposterior left, chronic ischemic bilateral white matter changes and with changes typical for encephalitic neuroinflammation changes located in cingulated and superior frontal gyrus (widened cingulated and superior frontal gyrus hypointense on T1w, hyperintense on T2w and FLAIR sequences, with diffusion restriction left and mild postcontrast opacification). Limbal punction was performed and analyses showed no signs of neuro infection. This case report could widen the knowledge of this complex disease and provide useful information, bringing a new vision about a possible topography causing such complex clinical presentation and referencing to clinicians of different specialties (radiologists, neurologists, clinical pharmacologists, internists, etc.) so that diagnosis and treatment for patients with similar clinical manifestations could be promptly recognized.
The term autoimmune encephalitis (AE) nominates a broad spectrum of immune-mediated diseases (inflammation caused by antibodies, and reactions they produce) in the central nervous system (CNS), located most commonly anatomically in the mesial temporal lobe and limbic system (the involvement of the striatum, diencephalon, or rhombencephalon can also be seen), that share overlapping clinical features and neuroimaging findings but are ultimately sub differentiated by the specific antibody subtypes driving the underlying immune-mediated attack on different CNS structures [1,2].
One of the AE classifications is into two broad categories: paraneoplastic or non-paraneoplastic, based on the presence of autoantibodies targeted to intracellular or neuronal cell-surface antigens (3). In general, antibodies against intracellular antigens are mediated through cytotoxic T-cell answer mechanisms; in these cases, neuronal damage comes across to be irrevocable, and bonds are found with underlying malignancies (most frequently with small-cell lung cancer, testicular cancers, and ovarian teratomas, and etc.), and poor response to immunotherapy and dismal prognosis, and structural abnormalities are not confined to the limbic anatomical structures [3]. Contrariwise, in constricted limbic encephalitis, neuronal cell-surface antigens are attacked targets, and an associated malignancy is uncommon, and usually in the absolute moiety of cases, responds more effectively to applied immunotherapy [4]. Main AE DDx is low-grade neoplasms, idiopathic inflammatory-demyelinating diseases (IID), acute disseminated encephalomyelitis (ADEM), anti-NMDAR encephalitis, limbic encephalitis (antibodies against AMPA receptor, GABA receptor or LGI1 protein), herpes virus encephalitis, etc. [5,6].
AE can be distinguished by certain recognizable features and lesion distribution on MR imaging, which include limbic encephalitis, cerebellar degeneration, striatal encephalitis, brainstem encephalitis, and ischemic periventricular leukoencephalopathy (leukoaraiosis) [3,4]. Endocranial MRI is a pivotal part of the acute encephalitis diagnostical process. It displays CNS signal abnormalities, especially contrast enhancement in postcontrast examinations, and reinforces a clinical suspicion of encephalitis, especially when the detection and pinpointing of the prime movers by lumbar puncture is deficient. Proper interpretative knowledge of the MRI patterns of CNS involvement can also be very helpful to neuroradiologists in suspecting a particular pathological driving force. However, MRI examinations must be interpreted in line with the clinical context (anamnesis, frailty, immunosuppression, positive data of recent travel in endemic areas), and should always integrate the DDx, mainly related to vascular, other infective, neoplastic, and/or inflammatory causes. MRI is, therefore, so to say a super-powerful diagnostic tool for brain infections (both initial diagnosis of the nature of the disease, and applied treatment monitoring), after analysis of the cerebrospinal fluid. Its technique must be complete, including the ‘‘functional’’ sequences (spectroscopy, DWI, DTI, for the DDx). From the above-mentioned reasons, it is clear and understandable that it is very useful to have a variety of antibodies as a clinical supplement to have precise classification and to avoid pigeonholing all encephalitis in a single group category [5,6] (Figure 1- Figure 6).

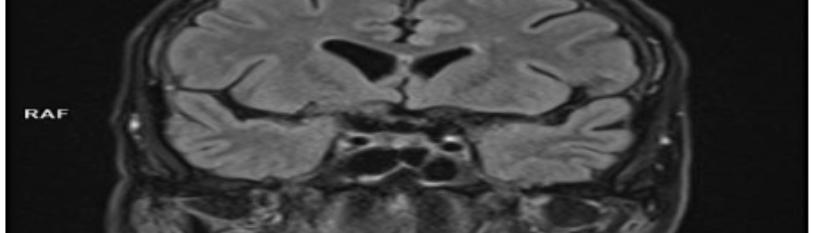
Figure 1: This figure represents the T2W sequence where we could notice a hyperintensity field of encephalitic neuroinflammation changes located in cingulated and superior frontal gyrus - widened cingulated and superior frontal gyrus with incipient cortical thickening hypointense on T1w, hyperintense on T2w and FLAIR sequence.
Figure 2: This figure represents the T2W dark-fluid sequence (FLAIR) where we could notice a hyperintensity field of encephalitic neuroinflammation changes located in cingulated and superior frontal gyrus - widened cingulated and superior frontal gyrus with incipient cortical thickening hypointense on T1w, hyperintense on T2w and FLAIR sequences.
Figure 3: This figure represents the T2W dark-fluid sequence (FLAIR) where we could notice a hyperintensity field of encephalitic neuroinflammation changes located in cingulated and superior frontal gyrus - widened cingulated and superior frontal gyrus with incipient cortical thickening hypointense on T1w, hyperintense on T2w and FLAIR sequences. One microangiopathic chronicle change could also be seen located in the right superior frontal gyrus.
Figure 4: This figure represents a diffusion-weighted (DWI) sequence where we could notice a region of hyperintensity (restriction diffusion field) with a decline of the apparent diffusion coefficient (ADC) on the ADC map in the anatomical position located in the cingulated and superior frontal gyrus.
Conclusion
Endocranial MRI is a pivotal part of the acute encephalitis diagnostical process (potentially a very serious disease with documented up to 70% or even more mortality rates and more than 90% morbidity rates in untreated HSV1 encephalitis). It displays CNS signal abnormalities, especially contrast enhancement in postcontrast examinations, and reinforces a clinical suspicion of encephalitis, especially when the detection and pinpointing of the prime movers by lumbar puncture is deficient. Proper interpretative knowledge of the MRI patterns of CNS involvement can also be very helpful to neuroradiologists in suspecting a particular pathological driving force. However, MRI examinations must be interpreted in line with the clinical context (anamnesis, frailty, immunosuppression, clinical physical examination, positive data of recent travel in endemic and tropical areas), and should always integrate the DDx, mainly related to vascular and other infective, neoplastic, and/or inflammatory causes. MRI is, therefore, so to say a super-powerful diagnostic tool for brain infections (both initial radiological diagnosis of the nature of the disease, and applied treatment monitoring), after optimal initial analysis of the CSF. Its technique must be complete, including the ‘‘functional’’ sequences (spectroscopy, DWI, SWI, DTI, ASL for the DDx) as well as hybrid imaging techniques (PET-CT, PET-MRI, etc.) Since the pathophysiology of the inflammatory process is also accessible to FDG PET imaging. From the above-mentioned reasons, it is clear and understandable that it is very useful to have a variety of antibodies as a clinical supplement to have precise classification and to avoid pigeonholing all encephalitis in a single group category.
References
- Granerod J, Ambrose HE, Walsh AL, Morgan D, Solomon T, et al. (2010) Causes of encephalitis and differences in their clinical presentations in England: a multicenter, population-based prospective study. Lancet Infect Dis. 10(12):835–44.
- Quist-Paulsen E, Kran A-MB, Dunlop O, Wilson J, Ormaasen V. (2013) Infectious encephalitis: a description of a Norwegian cohort. Scand J Infect Dis. 45(3):179–85.
- Tuzun E., Dalmau J. (2007) Limbic Encephalitis and Variants: Classification, Diagnosis and Treatment. The Neurologist. 13(5):261-71.
- Kelley BP, Patel SC, Marin HL. (2017) Autoimmune Encephalitis: Pathophysiology and Imaging Review of an Overlooked Diagnosis. AJNR AM J Neuroradiol. 38(6):1070-78.
- Steiner I, Budka H, Chaudhri A, Salonen O, Sainio K, et al. (2010) Viral meningoencephalitis: a review of diagnostic methods and guidelines for management: viral meningoencephalitis. Eur J Neurol. 17(8):999–1057.
- Sämann PG, Schlegel J, Müller G, Prantl F, Emminger C, et al. (2003) Serial proton MR spectroscopy and diffusion imaging findings in HIV-related herpes simplex encephalitis. AJNR Am J Neuroradio. 24(10):2015-9.