Autogenous Tooth Graft: An Overview and Meta-Analysis
Ansi Shayar*
BDS, PG Dip Implantology, UAE
*Corresponding author: Ansi Shayar, BDS, PG Dip Implantology, UAE.
Citation: Shayar A. (2023) Autogenous Tooth Graft: An Overview and Meta-Analysis. J Oral Med and Dent Res. 4(2):1-5.
Received: August 21, 2023 | Published: September 05, 2023
Copyright© 2023 Genesis Pub by Shayar A. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0). This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author(s) and source are properly credited.
DOI: https://doi.org/10.52793/JOMDR.2023.4(2)-42
Abstract
Graft materials are in use in dentistry to rehabilitate the bone loss which crop up in the oral cavity on various grounds, a few of which are periodontitis, traumatic tooth extraction, physiologic bone resorption, etc. During the process of prosthetic rehabilitation through dental implants or dentures alveolar bone resorption poses a perilous to the dentist, thus making it necessary to avail the grafting techniques using different graft materials to create the adequate bone volume.
Introduction
The grafts are generally restricted to four types depending on the scenario which are: 1. periodontal bone graft 2. Ridge augmentation 3. Socket preservation 4. Sinus lift. Any bone graft material used should provide mechanical support and stimulate osteo-regeneration. The factors which decide the choice of graft material for any bone grafting procedure depends on various the factors such as patient concerns, the type of surgical procedure, medical history and bone quality issues.
Characteristics of the Best Bone Graft Material for a Dental Implant are:
- Osteogenesis: living osteoblasts promote the formation of additional osteoblasts to form on the scaffolding.
- Osteoinduction: stimulating the migration of mesenchymal stem cells into the grafting site via blood vessels. The mesenchymal stem cells then stimulate undifferentiated osteoprogenitor cells to form osteoblasts.
- Osteoconduction: encouraging osteoblasts produced by the body to integrate within the graft structure, using it as a scaffold for new bone formation and repair.
An ideal graft material poses all of these characteristics which is autograft. Autograft has always been the Gold standard of ant grafting material available in the literature.
Graft materials are classified into 3 types based on their source of origin they are in Table 1:
|
Graft types |
Source |
Properties |
|
Autograft |
Own body |
Osteoinduction,osteoconduction, osteogenesis |
|
Allograft |
Human cadaver |
Osteoinduction, osteoconduction |
|
Xenograft |
Animal source |
osteoconduction, |
|
Alloplast |
Synthetic materials |
osteoconduction |
Table 1: Graft types and properties.
Graft types Source Properties
- Autograft Own body Osteoinduction, Osteoconduction, Osteogenesis
- Allograft Human Cadaver Osteoinduction, Osteoconduction
- Xenograft Animal Source Osteoconduction
- Alloplast Synthetic Materials Osteoconduction
The best graft material available is autograft which involves harvesting the bone from the patient’s own body .The morbidity associated with the donor site and the necessity of an additional surgery made the surgeons to find an alternative in partially edentulous patients using the patient’’s own tooth whch has to be extracted as part of the implant surgery and prosthetic rehabilitation. This method is called Autogenous tooth graft.
Autogenous dentin has been found to stimulate bone tissue formation and it provides a material with ideal physical and chemical properties .Physical properties include density, roughness and homogeneity Out of the 70 % inorganic content in human dentin, four types of calcium phosphate (hydroxyapatite, tricalcium phosphate, octacalcium phosphate, and amorphous calcium phosphate) attributes for the osteoconductive properties of it.
The hydroxyapatite in dentin is in the form of calcium phosphate with low crystal content, which makes it easily degradable by osteoclast activity. It is composed of 20 % organic content, of which 90 % is a type I collagen network and 10 % non-collagenous proteins (osteocalcin, osteonectin, sialoprotein, and phosphoprotein, which participate in bone calcification) and growth factors (bone morphogenetic proteins: BMPs, and insulin-like growth factor, which give the tooth osteoinductive properties); the remaining 10 % is water.
The extracted tooth is being converted into an amorphous mass of demineralised dentin using the machine and method specially designed for this technique. Many devices for tooth/dentin preparation have been described in the literature; among the articles reviewed here, the Smart Dentin Grinder was the most commonly used device, followed by the Tooth Transformer.
Histomorphometric examination was performed in 6 of the 11 studies; a percentage of vital new bone ranging from 20.78 % ± 13.29–66.5 % and a percentage of residual graft ranging from 0.9 % to 19.70 % ± 13.75 % were observed between 4 and 7 months after ARP.
Figure 1: Specimen preparation: (a) Example of the final specimens after enamel and cementum removal with a dental drill; (b) specimens in the sterile trituration chamber; (c) detail of Smart Dentin Grinder machine (KometaBio Inc., Cresskill, NJ, USA); (d) ground dentin with particle size less than 300 µm; (e) ground dentin with particle size between 300 µm and 1200 µm; (f) dentin particulate immersed in a sterile container with sterile saline solution.
In the case of severe volumetric bone loss, ridge augmentation has been made by using the custom-made TITANIUM mesh. The radiographs of the resorbed ridge has been super constructed with 3D technology and the super imposed images has been used to make the titanium mesh prior to the surgery .On the day of surgery the dentin particles are stabilised with the titanium mesh and fixed with mini screws. After 6 months the patient has been recalled and the titanium mesh removed achieving ossseointegration with no bone loss. Then on the second stage the Implant has been placed on the augmented bone. The clinical analysis of one case done in UAE gave this report.
The below image (source https://www.nature.com/articles/s41368-020-00107-z) shows the demonstration of construction of super structure on resorbed ridge and customizing titanium mesh on the superimposed image which can be used at the time of surgery.
Figure 2: Histological analysis images after autogenous dentin placement.
Figure 3: Histologic analyses of 2-week biopsy sample. a) The new cell lining and attachment to Auto BT powder and b) Newly deposited osteoid formations were observed. (H&E staining, X 200).
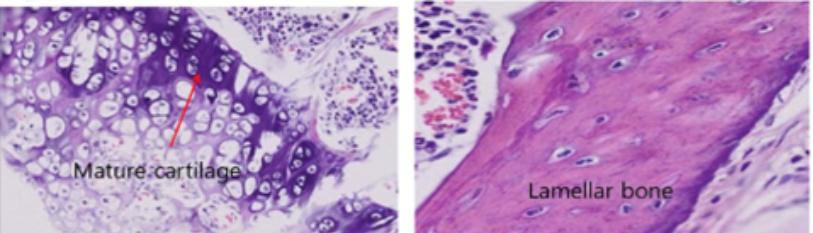
Figure 4: Cartilages were formed at the periphery of Auto BT in 5-week biopsy sample (H&E staining X 200).
Figure 5: a) Endochondral ossification and b) lamellar bone formation were identified 8 weeks after the insertion of Auto BT powder in the intramuscular pouch of athymic mice (H&E, staining, X 200).
Figure 6: Extracted teeth can be used as autoBT in 3 ways a): Extracted teeth. Foreign body such as prosthetic crown, cements, calculus, and soft tissue are removed. AutoBT is then fabricated through pulverization, defatting, demineralization, and lyophilization. b): AutoBT one-powder. Crown and root portion are mixed. c): AutoBT crown and root powder. d): AutoBT chips. e): AutoBT block.
Conclusion
A group of researchers in Seoul University made comparative retrospective studies on the histomorphologic studies about the AUTO BT graft and the results were satisfactory. Auto BT consisted of low-crystalline hydroxyapatite (HA) and other calcium phosphate minerals (ß-tricalcium phosphate (ß-TCP), ACP, and OCP). These are similar to the minerals of human bone tissues. But the level of HA crystallization and the amount of HA differs depending on the area of the tooth. The XRD pattern was much stronger in the crown portion with enamel than in the root. So, AUTO BT can be used safely in a variety of bone reconstructive procedures such as sinus bone graft, GBR, ridge augmentation and extraction socket graft. It is better than using allogenic and xenographic materials.
References
- Kim YK, Lee JK, Kim KW, Um IW, Murata M. (2013) Healing Mechanism and Clinical Application of Autogenous Tooth Bone Graft Material.
- Kim YK, Kim SG, Byeon JH, Lee HJ, Um IU. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 109(4):496-503.
- Orgeas GV, Clementini M, De Risi V, De Sanctis M. (2013) Surgical techniques for alveolar socket preservation: a systematic review. Int J Oral Maxillofac Implants. 28(4):1049-61.
- Busher D, Chappuis V, C Belser U, Chen S. (2017) Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000. 73(1):84-102.
- R.A. Wood, L Mealey B. (2012) Histologic comparison of healing after tooth extraction with ridge preservation using mineralized versus demineralized freeze-dried bone allograft. J Periodontol. 83(3):329-36
- Wu D, Zhou L, Lin J, Chen J, Huang W, et al. (2019) Immediate implant placement in anterior teeth with grafting material of autogenous tooth bone vs xenogenic bone. BMC Oral Health. 19(1):266.

